Malignant Effusion, Carcinomas
Donna M. Coffey, MD
Key Facts
Clinical Issues
˜ 30% of all body fluids are malignant effusions
Carcinomas account for > 95% of malignant effusions in adult patients
Diagnosis of malignancy in a body fluid is indicative of a high-stage tumor
Grim prognosis
Cytology is a cost-effective and accurate method for detecting malignancy in effusion with overall sensitivity of 58-71% and specificity close to 100%
Cytopathology
Key feature is presence of a dual population of tumor cells with background mesothelial and inflammatory cells
Malignant cells on cell block form tight clusters, papillae, or acini sometimes situated in an empty space or lacunae
Architecture and nuclear features on cytology preparations correlate with cell block findings and, in most cases, with histology of primary neoplasm
Top Differential Diagnoses
Benign effusions secondary to infections, therapy effect, trauma, or metabolic disorders have reactive mesothelial cells with atypia worrisome for malignancy
Differential diagnosis with malignant mesotheliomas requires a panel of immunohistochemical stains
Poorly differentiated carcinomas can shed in a dispersed single cell pattern resembling large cell lymphomas
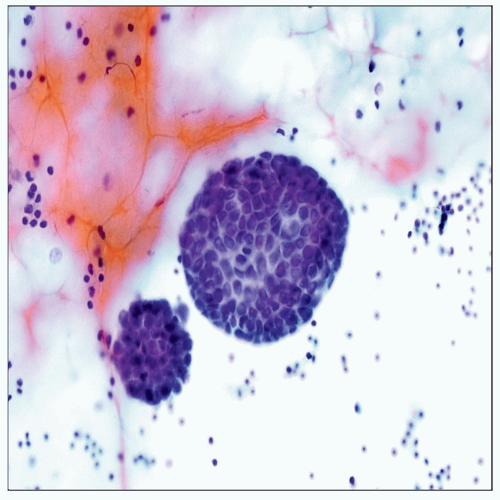 Pap stain of pleural fluid shows dense spherical groups or morulae of metastatic ductal adenocarcinoma. Clusters and spheres of metastatic adenocarcinoma have smooth cell borders. |
CLINICAL ISSUES
Presentation
˜ 30% of all body fluids are malignant effusions
Carcinomas account for > 95% of malignant effusions in adult patients
Most patients have a known primary neoplasm or multiple primary tumors
Malignant effusion is the 1st manifestation of an occult primary in up to 17% of patients
Cytology is a cost-effective and accurate method for detecting a malignancy in an effusion
Sensitivity for diagnosing malignancy ranges 58-71%
Repeated taps increase detection rate by almost 30%
Specificity of cytologic diagnosis is almost 100%
Rate of false-positive diagnosis is < 1%
Most occur in cases with marked mesothelial cell atypia
Adenocarcinomas account for 60-65% of pleural and pericardial and 80% of peritoneal malignant effusions
Breast cancer: Most common primary in malignant pleural/pericardial effusions in females
Lung cancer: Most common primary in malignant pleural/pericardial effusions in males and 2nd most common in females
Squamous cell carcinomas account for 2-4% of all malignant effusions
Most are poorly differentiated carcinomas from lung, cervix, or esophagus
Small cell carcinomas account for 4% of pericardial and 2-9% of malignant pleural effusions
Prognosis
Diagnosis of malignancy in a body fluid is indicative of a high-stage tumor with poor prognosis
Median survival for patients with a positive effusion is < 6 months
CYTOPATHOLOGY
Cellularity
Malignant effusions are usually highly cellular
Cellularity persists in repeated taps
Pattern
Adenocarcinomas exfoliate as large cohesive clusters or spheres with smooth cell borders, papillary fragments, or dispersed single cells
Squamous cell carcinomas present as single cells, sheets, or cohesive clusters
Small cell carcinomas exfoliate as single cells, short chains, or small tight clusters of tumor cells
Background
Variable amount of inflammatory cells ± necrotic debris
Background mucin and foamy macrophages in cases of pseudomyxoma peritonei
Psammoma bodies can be seen in carcinomas with papillary architecture (i.e., ovarian serous carcinoma, lung, thyroid, mesotheliomas)
Psammoma bodies are not diagnostic of malignancy as they can also be seen in endosalpingiosis or mesothelial hyperplasia
Squamous and small cell carcinomas often have karyorrhectic debris
Anucleated squamous cells are often present in squamous cell carcinomas
Cells
Most cases display obvious malignant features with pleomorphic cells, high nuclear:cytoplasmic ratio, irregular nuclear membranes, irregular chromatin distribution, and prominent nucleolus
Breast carcinoma, ductal type: Dense spherical groups/morulae, clusters, or single cells
Lobular carcinoma: Single cells, short chains, or clusters of small hyperchromatic cells with high
nuclear:cytoplasmic ratio and intracytoplasmic mucin droplets
Immunohistochemical (IHC) stains for diagnosis/biomarkers: BRST-2, mammaglobin, ER, PR, and HER-2/neu
Lung carcinoma: Variable architectural patterns, including papillary groups, clusters, sheets, and single cells
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



