Lymphoid Aggregates in Bone Marrow
Kaaren K. Reichard, MD
Key Facts
Etiology/Pathogenesis
Seen with increasing age; patients often female
Associated with infection, autoimmune disease, immune dysregulation
Microscopic Pathology
Reactive LAs usually few in number
Small, nodular, nonparatrabecular
Well circumscribed
Composed mostly of small lymphocytes
May see plasma cells, histiocytes
Morphologic variations
Germinal center formation, atypical cells, lipogranulomas, epithelioid histiocytes
Ancillary Tests
Immunophenotyping
Predominance of T cells (CD3) or equal admixture of T and B cells (CD20) by immunohistochemistry
No abnormal B- or T-cell population by flow cytometry
No aberrant antigen expression
Top Differential Diagnoses
Nodular lymphomas/leukemias
May distinguish by morphology &/or immunophenotyping
Predominance of CD20(+) B cells in B-cell lymphoma
Distinctive paratrabecular pattern in follicular and mantle cell lymphoma
Aberrant antigen expression
Typical neoplastic cells in classical Hodgkin lymphoma
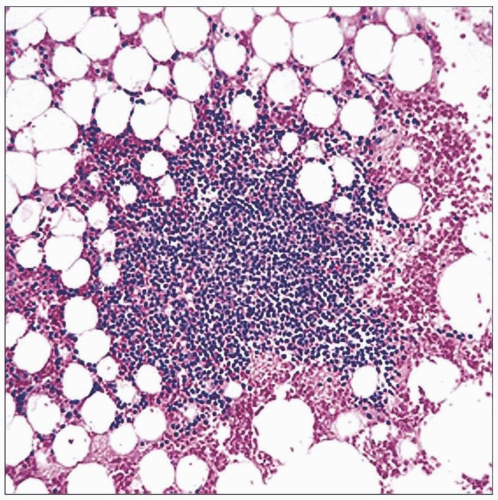 This is the typical appearance of a benign lymphoid aggregate in bone marrow; it is nodular, nonparatrabecular, well circumscribed, and composed of predominantly small mature lymphocytes. |
TERMINOLOGY
Abbreviations
Lymphoid aggregate (LA)
Bone marrow (BM)
Definitions
Focal collections of nonneoplastic lymphoid cells
Usually identified in BM clot and core biopsy sections
ETIOLOGY/PATHOGENESIS
Infectious Agents
Variety of systemic infections may be associated with benign LAs in bone marrow
Viral most common (e.g., HIV, Epstein-Barr virus)
Underlying Immune Disorders
Autoimmune disorders
Collagen vascular disease
CLINICAL ISSUES
Epidemiology
Incidence
Increases with age
Age
More common in older individuals
Gender
Tends to be more common in females
Presentation
Asymptomatic
If symptomatic, relates to underlying disorder
Laboratory Tests
Performed for work-up of possible underlying etiology
Systemic infection
Autoimmune disorder
Neoplasia
Treatment
No treatment necessary for benign LAs per se
Treatment targeted toward underlying disease (e.g., infection, immune dysregulation)
Prognosis
Relates to underlying disease
MICROSCOPIC PATHOLOGY
Histologic Features
Small, round, well circumscribed, interstitial/nonparatrabecular
Morphologic variations
Large, polymorphous aggregates (e.g., HIV)
Occasional larger atypical or activated cells (e.g., infection, autoimmune disorder)
Associated germinal center (occasional)
Associated lipogranuloma (especially in elderly)
Associated histiocytes
Cytologic Features
Round or slightly irregular nuclear contours, mature, clumped chromatin, inconspicuous nucleoli, usually scant cytoplasm
Predominant Pattern/Injury Type
Circumscribed
Focal, nodular
Interstitial
Perivascular
Predominant Cell/Compartment Type
Lymphocyte
Bone Marrow Aspirate
Bone Marrow Clot Section/Core Biopsy
Discrete foci of predominantly small lymphocytes
Interstitial/nonparatrabecular distribution, perivascular, adjacent to dilated sinuses, or associated with a small, penetrating vessel
Morphologic variations
Large, poorly circumscribed, polymorphous infiltrates
Typical of human immunodeficiency virus infection
Often see admixed larger, atypical cells; may require distinction from lymphoid neoplasia
Occasional larger atypical or activated cells
Typical of infection or ongoing immune reaction
Associated germinal center
Uncommon overall
More evident in autoimmune disorders
Associated with lipogranuloma
Associated with small collections of epithelioid histiocytes
ANCILLARY TESTS
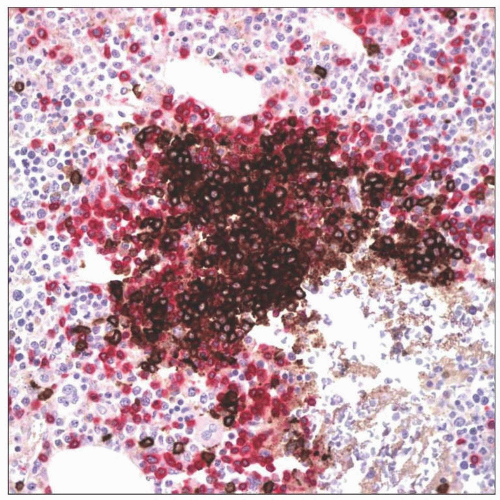
Immunohistochemistry
Cellular composition
Predominance of CD3(+) T cells with few admixed CD20(+) B cells or
Equal admixture of CD20(+) B cells and CD3(+) T cells
Cellular distribution
B cells tend to locate centrally surrounded by concentric rim of T cells
B-cell antigen expression
No aberrant detection of CD5, CD10, CD43
Normal germinal center cells may be CD10(+)
Flow Cytometry
Polyclonal B cells
Normal T-cell antigens and subsets
Caveat
Lymphoid aggregate cells may not be well represented in flow cytometric BM aspirate samples
Genetics
Nonclonal
DIFFERENTIAL DIAGNOSIS
Lymphomas/Chronic Leukemias with Nodular Pattern
General comments
Paratrabecular or intrasinusoidal pattern helps distinguish from benign LAs
B-cell disorders show B-cell predominance (CD20/CD19)
Reed-Sternberg cells in classical Hodgkin lymphoma
Aberrant antigen expression
CD5(+) in chronic lymphocytic leukemia (CLL) and mantle cell lymphoma (MCL)
CD10(+) in follicular lymphoma
Cyclin D1(+) in MCL
Light chain restriction by flow cytometry
Molecular studies
Clonal
Recurring genetic abnormalities in certain disorders [e.g., t(11;14)(q13;q32) in MCL]
After rituximab (anti-CD20) treatment
Post-therapy aggregates are T-cell predominant
Useful distinguishing features from benign LAs
Often paratrabecular
Often poorly circumscribed
CD79a and CD19 useful to identify residual neoplastic cells
Hematogones
Rarely cluster
Characteristic immunophenotypic profile
Metastatic Tumor
In addition to nodular collections, also tend to see sinusoidal involvement
Cells typically much larger than lymphocytes
Lymphoid markers are negative (e.g., CD20, CD3)
Express tumor-associated antigens
Erythroid Colonies
Foci of erythroid precursors (round, often dark nuclei) may mimic lymphoid aggregates
Often result of poor processing, sectioning, staining
Cells are negative for lymphoid markers; positive for hemoglobin A
DIAGNOSTIC CHECKLIST
Pathologic Interpretation Pearls
Morphologic appearance
Nodular, nonparatrabecular; may also be perivascular or adjacent to dilated sinus
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree