Lymphoblastic Lymphoma
Key Facts
Etiology/Pathogenesis
Neoplastic proliferation of blastic precursor lymphocytes
Clinical Issues
Occurs more commonly in children than in adults
Anterior superior and middle mediastinum
Rapidly enlarging mediastinal mass
Aggressive clinical course
Microscopic Pathology
Diffuse sheets of immature lymphoid cells
Infiltration of lymph node capsule and mediastinal fat with “single file” arrangement of tumor cells
“Starry sky” appearance due to numerous tingible body macrophages
Crush artifact
Lymphoblasts show large immature nuclei with dense chromatin and small inconspicuous or absent nucleoli
Lymphoblasts can be convoluted or nonconvoluted
Almost all precursor lymphocytes (T and B) express nuclear enzyme, terminal deoxynucleotidyl transferase (TdT)
Precursor lymphocytes also express CD34 and CD99
Top Differential Diagnoses
Burkitt lymphoma
B-cell chronic lymphocytic leukemia/small lymphocytic lymphoma
Lymphocyte-rich thymoma (WHO type B1)
Most important test is immunoperoxidase stain for pancytokeratin to identify scattered neoplastic thymic epithelial cells
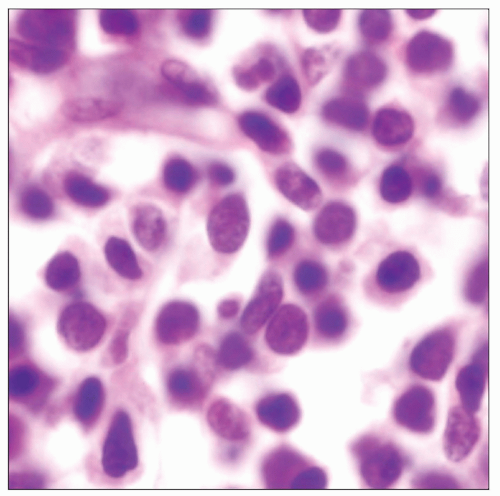 High magnification of nonconvoluted T-lymphoblastic lymphoma of the mediastinum shows primitive nuclei with dense chromatin pattern and with smooth nuclear contours. |
TERMINOLOGY
Abbreviations
Lymphoblastic lymphoma (LBL)
Synonyms
Lymphoblastic lymphoma/leukemia, lymphoma of precursor lymphocytes
Definitions
Diffuse lymphoma of immature or precursor lymphocytes, predominantly of T-cell type
ETIOLOGY/PATHOGENESIS
Pathogenesis
Neoplastic proliferation of blastic precursor lymphocytes
Associations with prior radiation, Down syndrome, and other genetic diseases have been noted
Phenotype can be either of T-precursor cell type or B-precursor cell type
CLINICAL ISSUES
Epidemiology
Incidence
Occurs more commonly in children than in adults
Incidence in children is about 3 cases per 100,000 population
75% of affected children are under 15 years of age
Peak incidence in children is between 2-5 years old
More frequent in males than females
Also affects men in 3rd decade of life
Can rarely occur in older individuals over age of 60 years
Site
Anterior superior and middle mediastinum
Supradiaphragmatic, supraclavicular, cervical, and axillary lymph nodes
Presentation
Rapidly enlarging mediastinal mass
Aggressive clinical course
Rapid progression, often with superior vena cava syndrome
Frequent relapses
Short survival
Generally diagnosed in advanced stages (stage III or IV)
Dissemination to other organs is common
Central nervous system (most common site of relapse)
Skin, testes, eyes, kidneys, breast, and lungs
Bone marrow involvement occurs early in disease
Leukemic phase with circulating blasts in peripheral blood occurs shortly after initial diagnosis
IMAGE FINDINGS
General Features
Location
Superior mediastinal nodes (prevascular and paratracheal)
Radiographic Findings
Bulky mediastinal bilateral hilar lymphadenopathy
Pleural effusion may be seen due to lymphatic or venous obstruction
CT Findings
Contrast-enhanced computed tomography (CECT) is imaging modality of choice
Slight to moderate uniform enhancement following intravenous contrast
MICROSCOPIC PATHOLOGY
Histologic Features
Diffuse sheets of immature lymphoid cells
“Pseudonodular” pattern due to compartmentalization by thin strands of fibrous tissue
Infiltration of lymph node capsule and mediastinal fat with “single file” arrangement of tumor cells
“Starry sky” appearance due to numerous tingible body macrophages
Crush artifact
Occasional spared, residual lymphoid follicles with germinal centers may become entrapped by lymphoblastic proliferation
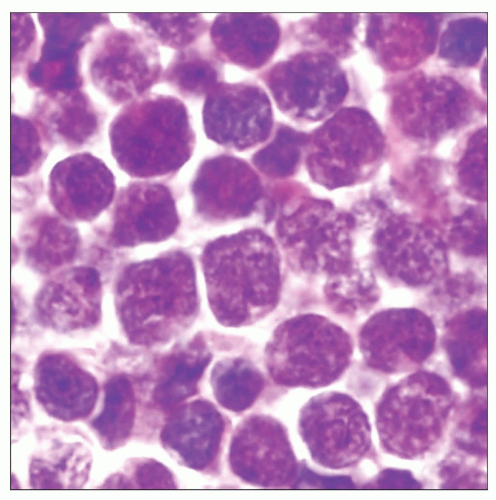
Cytologic Features
Lymphoblasts show large immature nuclei with dense chromatin and small, inconspicuous or absent nucleoli
Lymphoblastic cells show high nuclear-to-cytoplasmic ratio
Lymphoblasts can be convoluted or nonconvoluted
Convoluted lymphoblasts show multiple, complex nuclear indentations
Nonconvoluted lymphoblasts show smooth nuclear contours
Frequent mitotic figures
ANCILLARY TESTS
Immunohistochemistry
Almost all precursor lymphocytes (T and B) express the nuclear enzyme terminal deoxynucleotidyl transferase (TdT)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree