Lymph Nodes, Axillary: Diagnosis
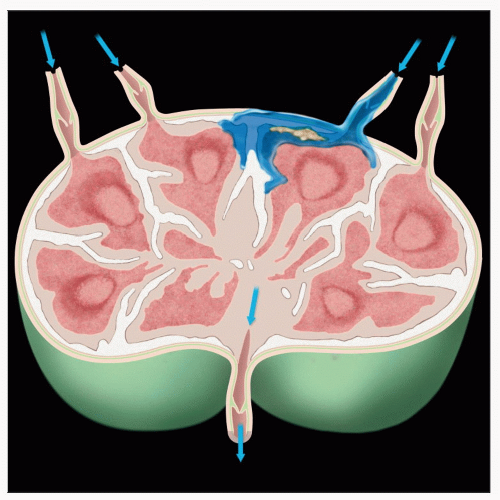 Afferent lymphatics enter the node in a central plane. Bisecting the node in this plane is most likely to reveal metastasis. Macrometastases should be detectable regardless of the plane of section. |
SURGICAL/CLINICAL CONSIDERATIONS
Goal of Consultation
Determine if macrometastatic (≥ 2 mm) carcinoma is present in sentinel lymph node(s)
Metastases < 2 mm may or may not be detected
Change in Patient Management
If metastasis is present, additional lymph nodes may be excised
If no additional surgery is planned, there is no need for intraoperative evaluation of lymph nodes
Clinical Setting
In the past, decisions concerning systemic therapy for breast cancer relied heavily on nodal status
Systemic therapy vs. no systemic therapy
Chemotherapy vs. hormonal therapy alone
Currently, molecular type of breast cancer is more commonly used for these decisions
Well- or moderately differentiated estrogen receptorpositive cancers with a low proliferative rate are generally treated with hormone therapy alone
Poorly differentiated estrogen receptor-negative or HER2-positive cancers are generally treated with chemotherapy
Nodal status is predictive of survival but not response to therapy; therefore, nodal sampling may not be necessary in some patients
Some patient groups as defined by the ACOG Z0011 trial may not undergo axillary dissection if only 1 or 2 sentinel nodes are positive
SPECIMEN EVALUATION
Gross
All nodes are carefully bluntly dissected from specimen and counted
Number of nodes present and with metastases are used to determine need for additional surgery
If there is a gradient of blue dye, metastasis is most likely to be at the blue-stained pole
Each node is thinly sliced at 2 mm intervals
All slices of all nodes are frozen
If there is a grossly evident metastasis, only 1 representative section need be frozen
Scrape or touch preparation can also be used to document grossly positive lymph node
If node is grossly suspicious for lymphoma or granulomatous disease, preservation of nonfrozen tissue is helpful for ancillary studies
Flow cytometry, frozen tissue (molecular studies), and hematopathology fixatives for suspected lymphoma
Cultures for granulomatous disease
If each node is inked a different color, slices from > 1 node can be frozen in same block
It is important to be able to count number of nodes with metastasis
Radioactive nodes detected with usual techniques employed do not expose pathology personnel to dangerous levels of radiation
Special protective equipment is not required
Special storage or disposal of tissue or equipment are not necessary
If new or nonstandard technique is utilized, levels of radiation and resulting risk should be assessed
Handling procedures should be approved by institutional radiation safety office
Frozen Section
All slices of all nodes are frozen
At least 1 H&E slide including a complete cross section of all slices is evaluated
Cytology
Each cut surface is scraped with a curved scalpel blade or glass slide and smeared on another slide
Each node should be separately evaluated
Useful when either infection or lymphoma are suspected
Touch imprints, rather than scrape preparations, may be more helpful for lymphoma
RT-PCR
This technique has been proposed as an alternative to frozen section evaluation
Does not clearly distinguish metastases by size
False-negative results can occur
Some cases due to failure of carcinoma to express transcripts used for assay
False-positive results can occur
Transcription of mRNA from nontumor cells can occur
Contamination of specimens by nonmalignant epithelial cells is a concern
If large portions of tissue are taken (e.g., using 1/2 a node for assay), macrometastases may not be seen by histology
It may be impossible to distinguish a false-positive from a true-positive
Clinical significance of cases with positive RT-PCR result and negative result by histology is unclear
Node could have no tumor cells, isolated tumor cells, micrometastasis, or missed macrometastasis
REPORTING
Frozen Section
Presence or absence of metastases
Extranodal invasion, if present
Presence or absence of other pathologic processes
Number of positive and negative nodes
Size of lymph node metastases
Cytology
Number of positive nodes with estimated gross size of metastasis, number of negative nodes
MOST COMMON DIAGNOSES
Metastatic Breast Carcinoma
Most common carcinoma found in axillary nodes of women
If a blue dye gradient is present, metastasis is usually present at blue pole
Ductal and lobular carcinoma are most common variants
Metastatic tumor often resembles primary
Preoperative review of slides or reports can be very helpful for correlation
If metastatic tumor and primary are dissimilar, consider alternative diagnoses (e.g., benign inclusions or metastases from other sites)
Metastatic grade I and II lobular carcinomas can be very difficult to identify in nodes
Metastases may be focal
Usually present adjacent to peripheral subcapsular sinus
Rare metastases are present in center of node
Metastases (particularly from lobular carcinoma) may resemble reactive processes
Lymphoma
Would be an unusual and unexpected finding in axillary nodes of a woman with breast cancer
Women with known low-grade lymphoma/chronic lymphocytic leukemia may have nodal involvement
Cytologic preparations are helpful to reveal morphology and dyscohesive nature of cells
If sufficient tissue is available, tissue should be saved for special studies
Frozen tissue (DNA analysis)
Flow cytometry
Fixatives for hematopathology
If Hodgkin lymphoma or diagnoses other than lymphoma are possible, tissue should also be fixed in formalin
Melanoma
Tumor cells usually appear dyscohesive with markedly pleomorphic nuclei
Tumors that are pigmented grossly or microscopically are easy to identify
However, many metastatic melanomas do not exhibit obvious melanin production
Patients usually have well-known history of melanoma
In rare cases, metastatic melanoma to breast can be mistaken for a primary breast carcinoma
Sarcoidosis
Rarely involves axillary lymph nodes
Node is occupied by confluent noncaseating granulomas
Infection should be excluded by sending tissue for culture
Benign Inclusions
Usually look like well-formed tubules
Myoepithelial cells may be present
Breast stroma may or may not be present
May show apocrine or squamous metaplasia
Endosalpingiosis is present as single-layered tubules
Cells may be ciliated
Prior biopsies of benign or malignant papillary lesions can result in dispersal of papillary fragments in lymphatic and lymph nodes
Usually present as small cohesive clusters
Immunoperoxidase studies may be required for final classification
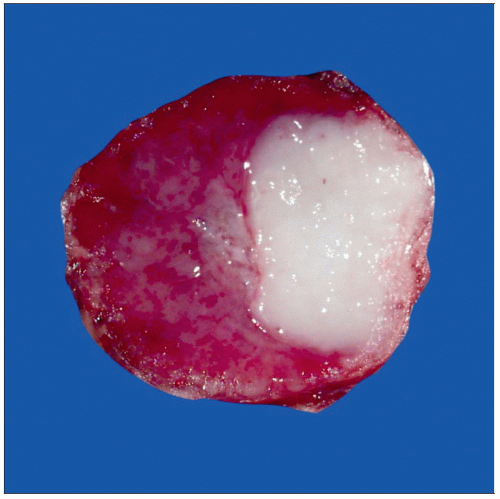
Silicone
Can seep out of implants (“bleed”) or be released when implant is ruptured
Can be transferred to regional lymph nodes
Silicone granulomas can be very hard and gritty when cut
Gross appearance and texture can closely mimic metastatic carcinoma
Silicone fills histiocytes
Silicone and metastatic carcinoma can be present in same lymph node
PITFALLS
False-Negative Diagnoses
Failure to examine entire node
If not all slices are frozen, macrometastases can be missed in ˜ 30% of cases
Tissue should never be taken from negative nodes in a way that would interfere with detecting all macrometastases
This includes tissue taken for alternative techniques such as RT-PCR
Metastatic lobular carcinoma
Can be very difficult to detect in frozen sections or in cytologic preparations
Single cell infiltrative pattern
Scattered throughout node rather than predominantly in peripheral sinuses
Tumor cells can resemble normal cells in lymph nodes
Grade I carcinomas resemble lymphocytes
Grade II carcinomas resemble histiocytes
Grade III carcinomas have nuclear pleomorphism and are generally easily recognizable
Signet ring cells with mucin vacuoles are helpful to recognize tumor cells
However, signet ring cells are not always present
Immunoperoxidase studies for keratin on permanent sections are necessary in some cases for final diagnosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree