Lymph Node Dissections of the Neck
Anuradha R. Bhama
Geeta Lal
Neck dissections encompass a wide variety of terminology and procedures. Each operation is tailored to the illness and the suspected degree of metastasis. It is essential to have an understanding of the levels of the lymph nodes in the neck to grasp the surgical variations. The classic radical neck dissection entails en bloc resection of all soft tissues bordered superiorly by the inferior aspect of the mandible, inferiorly by the clavicle, medially by the midline of the neck, and posteriorly by the trapezius muscle.
A modified radical neck dissection differs from a radical neck dissection in that it preserves one or more structures, namely the sternocleidomastoid (SCM) muscle, the spinal accessory nerve, and the internal jugular vein. The modified radical neck dissection has largely replaced radical neck dissections because of improved cosmetic and functional results with minimal morbidity and less than 1% risk of mortality.
Selective neck dissection and “berry picking” respectively refer to operations in which the surgeon has chosen to remove an isolated compartment or only those nodes that are clinically positive. Berry picking is generally not recommended at an initial operation because of the high rate of compartment recurrence. A central neck dissection refers to a neck dissection of level VI nodes in the paratracheal, paraesophageal, and upper mediastinal regions. It is typically performed for carcinoma of the thyroid and may include resection of level VII or upper mediastinal nodes.
Complications after neck dissection primarily include nerve injury, hypoparathyroidism, and wound complications including seroma, hematoma, infection, and chyloma. A rare complication of bilateral neck dissection is the syndrome of inappropriate antidiuretic hormone.
This chapter begins with the standard radical neck dissection and then presents the common types of modified radical neck dissection and central neck dissection. Selective node dissection is also briefly discussed.
SCORE™, the Surgical Council on Resident Education, classified modified neck dissection as a “COMPLEX” procedure.
STEPS IN PROCEDURE
Standard or Modified Radical Neck Dissection
Position patient with head turned to contralateral side and elevate head of table slightly
Avoid placing incision in a line directly over carotid artery
Elevate flaps at level just deep to platysma
Identify and ligate facial artery and facial vein
Identify and protect marginal mandibular branch of facial nerve
Begin at inferior margin of field
Ligate and divide external jugular vein
If standard neck dissection:
Divide and elevate sternocleidomastoid muscle (may preserve for modified)
Identify, ligate, and divide internal jugular vein (may preserve for modified)
Elevate all surrounding fatty tissues with the divided structures, preserving underlying nerves
Terminate dissection at cephalad aspect, including submandibular gland with specimen
Meticulous closure, with closed-suction drains if desired
Selective Node Dissection
Generally, smaller incision—tailored to node group to be removed
En bloc selective removal of one or more groups of lymph nodes
Generally surrounding structures are preserved
Central Node Dissection
Generally done through a collar (thyroid) incision
Elevate subplatysmal flaps
Divide strap muscles in midline
Begin dissection at inferior aspect of field, resecting thymus
Skeletonize trachea and fatty tissues along esophageal groove to hyoid
Preserve recurrent laryngeal nerves
Preserve superior parathyroid glands
HALLMARK ANATOMIC COMPLICATIONS
Injury to Regional Nerves
Ansa cervicalis
Spinal accessory nerve
Hypogastric nerve
Vagus nerve
Recurrent laryngeal nerve
Injury to parathyroid glands (central neck dissection)
Blowout of carotid artery (delayed)
LIST OF STRUCTURES
Cricoid cartilage
Strap Muscles
Sternothyroid muscle
Omohyoid muscle
Sternohyoid muscle
Anterior jugular veins
Sternocleidomastoid muscle
Ansa cervicalis
Carotid Sheath
Carotid artery
Vagus nerve
Internal jugular vein
Digastric muscle
Spinal accessory nerve
Hypogastric nerve
Parotid Gland
Facial nerve
Innominate artery and vein
Thoracic inlet
Thymus
Thyrothymic ligament
Parathyroid glands, superior and inferior
Introduction
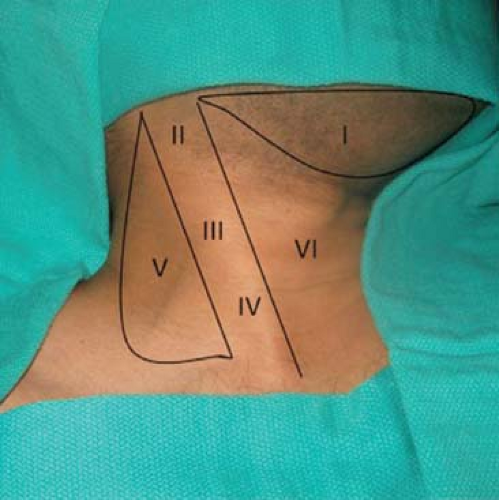
A critical understanding of the zones of the neck and tissue planes is necessary before performing a neck dissection. Lymph node classifications can be either by anatomic description or by levels of the neck. The named nodal groups include submental (level IA), submandibular (level IB), upper jugular (includes sublevels IIA and IIB), middle jugular (level III), lower jugular (level IV), posterior triangle group (includes sublevels VA and VB), and anterior compartment group (level VI). Level IA nodes lie within the boundaries of the anterior belly of the digastric and the hyoid bone. Level IB nodes lie within the boundaries of the anterior belly of the digastric, the stylohyoid muscle, and the body of the mandible. Levels II, III and IV are defined by the upper, middle, and lower third of the sternocleidomastoid (SCM). Level II is subdivided into IIA and IIB, based upon a vertical plane defined by the spinal accessory nerve. IIA nodes lie anteromedial to the plane, while IIB nodes lie posterolateral to the plane. Level V is subdivided into VA and VB by a plane defined by the level of the cricoid cartilage. VA lies superior to this horizontal plane, while VB lies inferior. Finally, level VI nodes are bound superiorly by the hyoid bone, inferiorly by the suprasternal notch, and laterally by the common carotid arteries. Level VI includes the pretracheal, precricoid (Delphian), and perithyroidal nodes (Fig. 11.1).
Standard Radical Neck Dissection
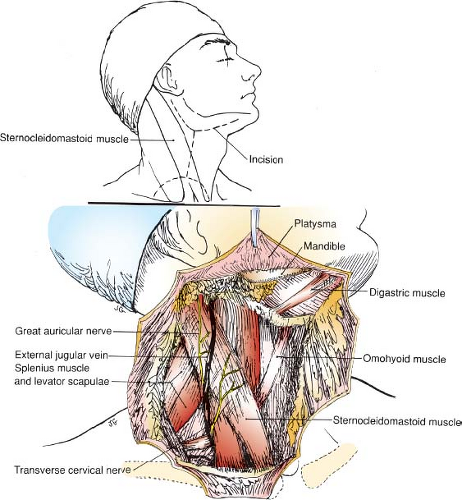
Incision and Development of Flaps (Fig. 11.2)
Technical Points
Position the patient supine with the neck in slight extension and the head turned slightly to the contralateral side. Prepare and drape a surgical field that includes the neck, lower face, and upper chest. Elevate the head of the table slightly to reduce venous bleeding.
A variety of incisions have been used for radical neck dissection. All involve elevation of flaps so that the entire area illustrated can be removed en bloc. Because many of these
patients have received radiation therapy, or may in the future undergo irradiation, viability of skin flaps is especially important. The H-shaped or double Y-shaped incision shown allows complete lymphadenectomy while preserving good, viable skin flaps. Alternative incisions are also illustrated.
patients have received radiation therapy, or may in the future undergo irradiation, viability of skin flaps is especially important. The H-shaped or double Y-shaped incision shown allows complete lymphadenectomy while preserving good, viable skin flaps. Alternative incisions are also illustrated.
Make an H-shaped incision, placing the vertical arm of the incision so that it does not lie directly over the carotid vessels. Make this limb of the incision vertical, rather than oblique, to place it away from the carotid sheath.
Identify the platysma and include it with the skin flaps as this improves blood supply to the skin flaps and greatly enhances the chances for their survival. Elevate the posterior flaps to the anterior border of the trapezius muscle, the superior flap to the mandible, the medial flap to the midline of the neck, and the inferior flap to the clavicle. The external jugular vein should be visible as it courses obliquely across the midportion of the SCM. As the flaps are raised, be careful to dissect in the adventitial plane of this vein.
At the superior border of the field, divide and ligate the facial (external maxillary) artery and facial vein. Identify the marginal mandibular branch of the facial nerve, which may be injured during the elevation of flaps. It generally is located parallel to and 1 to 2 cm below the lower border of the mandible, crossing superficial to the facial artery and facial vein. Gentle upward traction on the divided stumps of these vessels will retract the marginal mandibular branch safely up out of the field.
Anatomic Points
The platysma is innervated by the cervical branch of the facial nerve, which courses inferiorly deep to the platysma, with anterior branches supplying the platysma. The skin incision and the subsequent elevation of myocutaneous flaps will, of necessity, denervate all or part of the platysma.
The marginal mandibular branch of the facial nerve is important for cosmetic and functional reasons. This nerve innervates the muscles of the lower lip and chin and can lie as much as 2.5 cm inferior to the ramus of the mandible.
It is at risk during the development of the upper flap. Begin the incision to raise the superior myocutaneous flap at the mastoid process and then follow a gentle curve inferiorly, about 3 cm inferior to the posterior third of the ramus of the mandible. Then gently curve the incision superiorly and anteriorly to the mental protuberance of the chin.
It is at risk during the development of the upper flap. Begin the incision to raise the superior myocutaneous flap at the mastoid process and then follow a gentle curve inferiorly, about 3 cm inferior to the posterior third of the ramus of the mandible. Then gently curve the incision superiorly and anteriorly to the mental protuberance of the chin.
Branches of the great auricular nerve, a sensory branch of the cervical plexus bearing fibers from C2 and C3, will be severed during exposure of the upper attachment of the SCM. The vertical limb of the incision almost approximates the course of the external jugular vein, lying immediately deep to the platysma muscle. Be careful to identify this vein and keep the incision superficial to it. The incision also divides branches of the transverse cervical nerve, a sensory branch of the cervical plexus that also carries fibers of C2 and C3. The inferior limb of the incision is relatively risk-free. The supraclavicular nerves (sensory divisions of the cervical plexus carrying fibers of C3 and C4) that supply the skin of the lower neck and extend onto the upper thorax will be encountered and must be divided. The sensory branches of the cervical plexus all emerge from under the middle of the SCM and fan out from this point. Those that supply regions anterior to the SCM cross the superficial surface of that muscle. Several superficial veins will also be encountered deep to the platysma and should be controlled.
Dividing the Sternocleidomastoid Muscle and Beginning the Posterior and Inferior Dissection (Fig. 11.3)
Technical Points
Incise the fascia overlying the anterior border of the trapezius muscle to enter the posterior triangle of the neck. Ligate and divide the transverse cervical artery and vein at the lateral margin of the dissection. Sweep fatty and areolar tissues upward and medially. Identify the spinal accessory nerve, which may be sacrificed or preserved depending on individual preference and the degree of nodal involvement. This nerve is sacrificed in the classic radical neck dissection, but in practice, most surgeons preserve it.
Advance the incision medially, just above the clavicle, and, by sharp and blunt dissection, expose the external jugular vein. Ligate and divide this vein about 1 cm above the clavicle. Begin to sweep fatty and areolar tissues upward as the dissection progresses medially. Divide the posterior belly of the omohyoid muscle and the medial ends of the transverse cervical artery and vein, which run deep to the omohyoid muscle.
Incise the fascia medial to the SCM and gently elevate it, freeing the muscle from the underlying internal jugular vein. Divide the SCM from its attachments to the clavicle and sternum. Place a clamp on the divided stump of the SCM and use it to provide upward traction.
The brachial plexus, phrenic nerve, anterior scalene muscle, and internal jugular vein should be visible in the floor of the dissection.
Anatomic Points
The fascia investing the SCM, or the investing layer of the deep cervical fascia, also invests the trapezius muscle and the section of the spinal accessory nerve that passes from the SCM to the trapezius muscle. This nerve crosses the posterior triangle along a line running from slightly superior to the middle of the SCM to the anterior border of the trapezius muscle about 5 cm
superior to the clavicle. Some surgeons routinely sacrifice this nerve, while others sacrifice it only if it is directly invaded by tumor. Division of this nerve causes significant disability, as this potentially results in diminished trapezius muscle mass and partial paralysis of the trapezius and SCM.
superior to the clavicle. Some surgeons routinely sacrifice this nerve, while others sacrifice it only if it is directly invaded by tumor. Division of this nerve causes significant disability, as this potentially results in diminished trapezius muscle mass and partial paralysis of the trapezius and SCM.
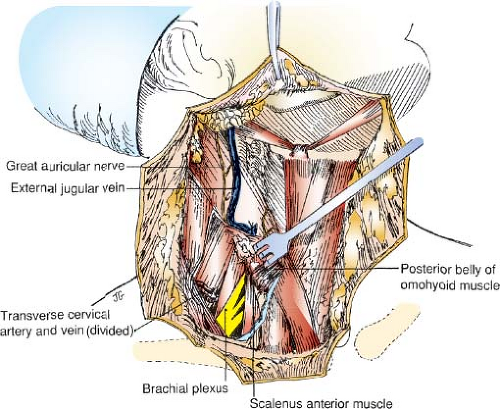 Figure 11.3 Standard radical neck dissection—dividing the sternocleidomastoid muscle and beginning the posterior and inferior dissection
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|