Lymph Node Dissections of the Neck
Laura A. Adam
Geeta Lal
Cervical neck dissections encompass a wide variety of terminology and procedures. Each operation is tailored to the illness and the suspected degree of metastasis. It is essential to have an understanding of the levels of the lymph nodes in the neck to grasp the surgical variations (see Fig. 11.1B). The classic radical neck dissection removes all soft tissues from the inferior aspect of the mandible to the midline of the neck to the clavicle and posterior to the trapezius muscle en bloc. A modified radical, or lateral, neck dissection refers to dissection of levels II through V. It differs from a radical neck dissection in that it spares the sternocleidomastoid muscle (SCM), spinal accessory nerve, and the internal jugular vein. The modified radical neck dissection has largely replaced radical neck dissection because of improved cosmetic and functional results with minimal morbidity and less than 1% risk of mortality. Selective neck dissection and “berry picking” respectively refer to operations in which the surgeon has chosen to remove an isolated compartment or only those nodes that are clinically positive. Berry picking is generally not recommended at an initial operation because of the high rate of compartment recurrence. A central neck dissection refers to a neck dissection of levels VI and VII, or those nodes in the paratracheal, paraesophageal, and upper mediastinal regions. It may be performed for carcinoma of the thyroid.
Complications after neck dissection primarily include nerve injury, hypoparathyroidism, and wound complications—including hematoma, infection, and chyloma. A rare complication of bilateral neck dissection is syndrome of inappropriate anti-diuretic hormone (i.e., SIADH).
This chapter begins with the standard radical neck dissection and then presents the common types of modified radical neck dissection and central neck dissection. Selective node dissection is briefly discussed at the end.
Steps in Procedure
Standard or Modified Radical Neck Dissection
Position patient with head turned to contralateral side and elevate head of table slightly
Avoid placing incision in a line directly over carotid artery
Elevate flaps at level just deep to platysma
Identify and ligate facial artery and facial vein
Identify and protect marginal mandibular branch of facial nerve
Begin at inferior margin of field
Ligate and divide external jugular vein
If standard neck dissection: divide and elevate sternocleidomastoid muscle (may preserve for modified, by mobilizing)
If standard neck dissection: identify, ligate, and divide internal jugular vein (may preserve for modified)
Elevate all surrounding fatty tissues with the divided structures, preserving underlying nerves
Terminate dissection at cephalad aspect, including submandibular gland with specimen
Meticulous closure, with closed suction drains if desired
Selective Node Dissection
Generally, smaller incision—tailored to node group to be removed
En bloc selective removal of one or more groups of lymph nodes
Generally surrounding structures are preserved
Central Node Dissection
Generally done through a collar (thyroid) incision
Elevate subplatysmal flaps
Divide strap muscles in midline
Begin dissection at inferior aspect of field, resecting thymus
Skeletonize trachea and fatty tissues along esophageal groove to hyoid
Preserve recurrent laryngeal nerves
Preserve superior parathyroid glands
Hallmark Anatomic Complications
Injury to Regional Nerves
Ansa cervicalis
Spinal accessory nerve
Hypogastric nerve
Vagus nerve
Recurrent laryngeal nerve
Injury to parathyroid glands (central neck dissection)
Blowout of carotid artery (delayed)
List of Structures
Cricoid cartilage
Strap Muscles
Sternothyroid muscle
Omohyoid muscle
Sternohyoid muscle
Anterior jugular veins
Sternocleidomastoid muscle
Ansa cervicalis
Carotid Sheath
Carotid artery
Vagus nerve
Internal jugular vein
Digastric muscle
Spinal accessory nerve
Hypogastric nerve
Parotid Gland
Facial nerve
Innominant artery and vein
Thoracic inlet
Thymus
Thyrothymic ligament
Parathyroid glands, superior and inferior
Standard Radical Neck Dissection
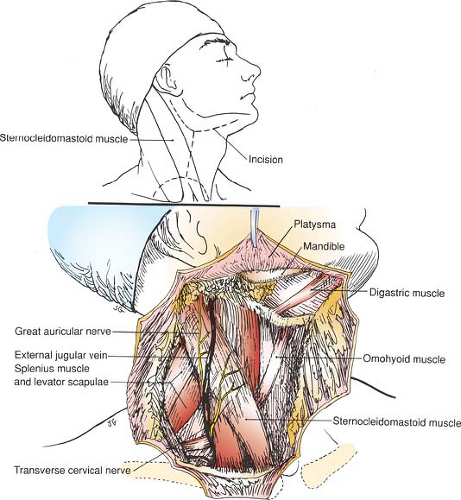
Incision and Development of Flaps (Fig. 11.1)
Technical Points
Position the patient supine with the neck in slight extension and the head turned slightly to the contralateral side. Prepare a surgical field that includes the neck, lower face, and upper chest. Elevate the head of the table slightly to reduce venous bleeding.
A variety of incisions have been used for radical neck dissection. All involve elevation of flaps so that the entire area illustrated can be removed en bloc. Because many of these patients have received radiation therapy, or may in the future undergo irradiation, viability of skin flaps is especially important. The H-shaped or double-Y-shaped incision shown allows complete lymphadenectomy while preserving good, viable skin flaps. Alternative incisions are also illustrated.
Make an H-shaped incision. Place the vertical arm of the incision so that it does not lie directly over the carotid vessels. Make this limb of the incision vertical, rather than oblique, to place it away from the carotid sheath.
Identify the platysma and include it with the skin flaps. This improves blood supply to the skin flaps and greatly enhances the chances for their survival. Elevate the posterior flaps to the anterior border of the trapezius muscle, the superior flap to the mandible, the medial flap to the midline of the neck, and the inferior flap to the clavicle.
The external jugular vein should be visible as it courses obliquely across the midportion of the SCM. As the flaps are raised, be careful to dissect in the adventitial plane of this vein.
At the superior border of the field, divide and ligate the facial (external maxillary) artery and facial vein. Look for and identify the marginal mandibular branch of the facial nerve. Injury to this nerve can occur when flaps are being elevated. It generally is located parallel to and 1 to 2 cm below the lower border of the mandible, crossing superficial to the facial artery and vein. Gentle upward traction on the divided stumps of these vessels will retract the marginal mandibular branch safely up out of the field.
Anatomic Points
The platysma is innervated by the cervical branch of the facial nerve. The nerve courses inferiorly deep to the platysma, with anterior branches supplying the platysma. The skin incision and the subsequent elevation of myocutaneous flaps will, of necessity, denervate all or part of the platysma.
The marginal mandibular branch of the facial nerve is important for cosmetic and functional reasons. This nerve innervates the muscles of the lower lip and chin and can lie as much as 2.5 cm inferior to the ramus of the mandible. It is at risk during development of the upper flap. Begin the incision to raise the superior myocutaneous flap at the mastoid process and then follow a gentle curve inferiorly, about 3 cm inferior to the posterior third of the ramus of the mandible. Then gently curve the incision superiorly and anteriorly to the mental protuberance of the chin.
Branches of the great auricular nerve, a sensory branch of the cervical plexus bearing fibers from C2 and C3, will be severed during exposure of the upper attachment of the SCM. The vertical limb of the incision almost approximates the course of the external jugular vein, lying immediately deep to the platysma muscle. Be careful to identify this vein and keep the incision superficial to it.
The incision divides branches of the transverse cervical nerve, a sensory branch of the cervical plexus that also carries fibers of C2 and C3.
The inferior limb of the incision is relatively risk free. The supraclavicular nerves (sensory divisions of the cervical plexus carrying fibers of C3 and C4) that supply the skin of the lower neck and extend onto the upper thorax will be encountered and must be cut. The sensory branches of the cervical plexus all emerge from under the middle of the SCM and fan out from this point. Those that supply regions anterior to the SCM cross the superficial surface of that muscle. Several superficial veins will also be encountered deep to the platysma and should be controlled.
Dividing the Sternocleidomastoid Muscle and Beginning the Posterior and Inferior Dissection (Fig. 11.2)
Technical Points
Incise the fascia overlying the anterior border of the trapezius muscle to enter the posterior triangle of the neck. Ligate and divide the transverse cervical artery and vein at the lateral margin of the dissection. Sweep fatty and areolar tissue upward and medially. Identify the spinal accessory nerve, which may be sacrificed or preserved depending on individual preference and the degree of nodal involvement. This nerve is sacrificed in the classic radical neck dissection, but in practice, most surgeons currently preserve it.
Advance the incision medially, just above the clavicle, and, by sharp and blunt dissection, expose the external jugular vein. Ligate and divide this vein about 1 cm above the clavicle. Begin to sweep fatty and areolar tissue upward as the dissection progresses medially. Divide the posterior belly of the omohyoid muscle and the medial ends of the transverse cervical artery and vein, which run deep to the omohyoid muscle.
Incise the fascia medial to the SCM and gently elevate it, freeing the muscle from the underlying internal jugular vein. Divide the SCM from its attachments to the clavicle and sternum. Place a Kocher clamp on the divided stump of the SCM and use it to provide upward traction.
The brachial plexus, phrenic nerve, anterior scalene muscle, and internal jugular vein should be visible in the floor of the dissection.
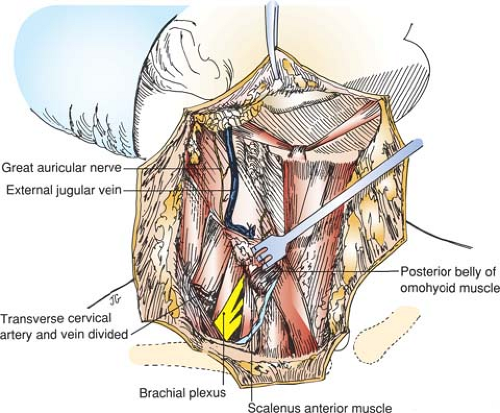 Figure 11-2 Standard Radical Neck Dissection—Dividing the Sternocleidomastoid Muscle and Beginning the Posterior and Inferior Dissection |
Anatomic Points
The fascia investing the SCM, or the investing layer of the deep cervical fascia, also invests the trapezius muscle and that part of the spinal accessory nerve that passes from the SCM to the trapezius muscle. Some surgeons routinely sacrifice this nerve, which crosses the posterior triangle along a line running from slightly superior to the middle of the SCM to the anterior border of the trapezius muscle about 5 cm superior to the clavicle. Others sacrifice it only if a tumor directly invades it. Division of this nerve causes significant disability because elevation, rotation, and retraction of the scapula are all affected, and atrophy of the trapezius muscle presents difficulties when a cervical collar is used.
The external jugular vein crosses the superficial surface of the SCM, passing inferiorly from its beginning in the parotid gland to its junction, just lateral to the clavicular attachment of the SCM, with the subclavian vein. The termination of the subclavian veins and the internal jugular veins is immediately deep to the SCM, as is the end of the thoracic duct on the left and its counterparts—the right lymphatic ducts—on the right.
The omohyoid muscle has two bellies. The inferior belly passes almost horizontally from its origin on the upper border of the scapula to the intermediate tendon (attached by a fascial sling to the medial ends of the clavicle and first rib), which intervenes between the SCM and the internal jugular vein. The superior belly passes superiorly, and almost vertically, to its attachment on the greater cornu of the hyoid. The inferior belly lies immediately superficial to the supraclavicular part of the brachial plexus, suprascapular and transverse cervical vessels, and phrenic nerve, which lies on the anterior scalene muscle. As the specimen is reflected craniad, the transverse cervical vessels are carefully ligated and divided. The phrenic nerve, crossed superficially by these vessels, must be identified and preserved. It lies deep to the lateral branches of the thyrocervical trunk and superficial to the anterior scalene muscle and is the only longitudinal structure coursing superolaterally to inferomedially in the lower neck.
Dissection in the Carotid Sheath and Ligation of the Internal Jugular Vein (Fig. 11.3)
Technical Points
By sharp and blunt dissection, open the carotid sheath and identify within it the internal jugular vein (Fig. 11.3A). Double-ligate and divide this vein just above the clavicle. Identify the vagus nerve and carotid artery lying posterior to the internal jugular vein. Sweep the internal jugular vein upward with the specimen protecting the vagus nerve and underlying carotid.
Dissection may then proceed relatively rapidly up along the carotid sheath until the carotid bifurcation is reached (Fig. 11.3B). Proceed slowly past the carotid bifurcation and identify and protect the hypoglossal nerve. This crosses the internal and external carotid arteries just above their bifurcation and then passes deep to the posterior belly of the digastric muscle.
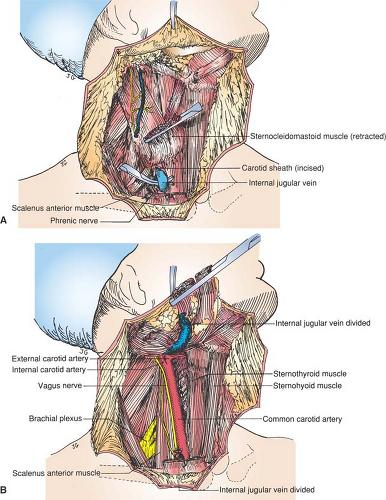 Figure 11-3 Standard Radical Neck Dissection—Dissection in the Carotid Sheath and Ligation of the Internal Jugular Vein |
The bed of the dissection should reveal the medial border of the trapezius muscle, the middle scalene muscle, and the levator scapulae muscle posteriorly (with the spinal accessory nerve, if preserved). The brachial plexus, phrenic nerve, vagus nerve, and common carotid artery should be visible and preserved in the floor of the dissection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree