Lymph Node Dissection in Thyroid Cancer
Gerard M. Doherty
DEFINITION
Most thyroid cancer develops from the follicular cells of the thyroid gland (differentiated thyroid cancer includes papillary and follicular subtypes).
Rare thyroid cancers develop from the C cells of the thyroid gland (medullary thyroid cancer).
Thyroid cancer of any subtype can be associated with lymph node metastases in the neck.
Clinical circumstances can indicate the need for cervical lymphadenectomy either as a therapeutic intervention for known metastases or as a prophylactic procedure for the diagnosis or therapy of occult metastases.
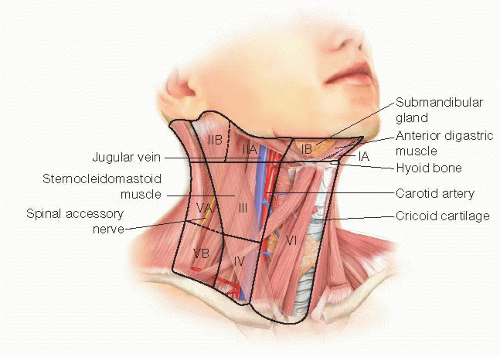
The lymph node compartments of the neck are divided into “levels” to allow communication of the affected and dissected areas (FIG 1).
Level 6 is also known as the central neck and includes the lymph nodes medial to the carotid sheath on each side and bounded by the hyoid bone superiorly and the sternum inferiorly.
Levels 1 through 5 are also known as the lateral neck and include all of the node compartments lateral to the carotid sheath on each side.
PATIENT HISTORY AND PHYSICAL FINDINGS
Thyroid cancer lymph node metastases can be palpable or, more often, nonpalpable but identifiable by imaging. Very small foci of thyroid cancer in lymph nodes may only be evident at microscopic pathology examination.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Patients with thyroid cancer should each have a staging ultrasound examination prior to operation.1 This allows mapping of the lymph node status of each compartment in the neck (FIG 2).
The level 6 lymph nodes are the most difficult to evaluate by ultrasound when the thyroid gland is still present, as these structures are in the same compartment.
Patients with large tumors or gross adenopathy may be best studied by computed tomography (CT) scan with contrast or magnetic resonance scanning, as these modalities allow better examination of the areas low in the neck that may be obscured by gross disease on ultrasound (FIG 3).
SURGICAL MANAGEMENT
Dissection of the level 6 lymph nodes is generally performed in conjunction with total thyroidectomy.
The level 6 lymph nodes are removed by clearing the soft tissue that surrounds the thyroid gland. No additional incision or mobilization is necessary.
Clearing these level 6 nodes involves additional manipulation of the soft tissue and vascular supply that surrounds the parathyroid glands. With these glands at additional risk of being damaged during operation, the performance of parathyroid autograft is particularly important to avoid permanent hypoparathyroidism2 (FIG 4).
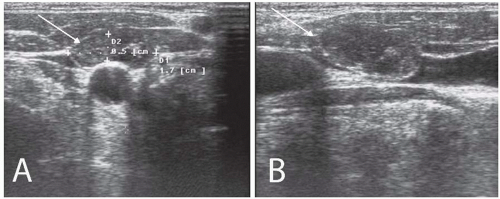 FIG 2 • Ultrasound demonstration of metastatic lymph nodes in thyroid cancer. Panel A shows a transverse view (arrow), and panel B shows the longitudinal view (arrow). |
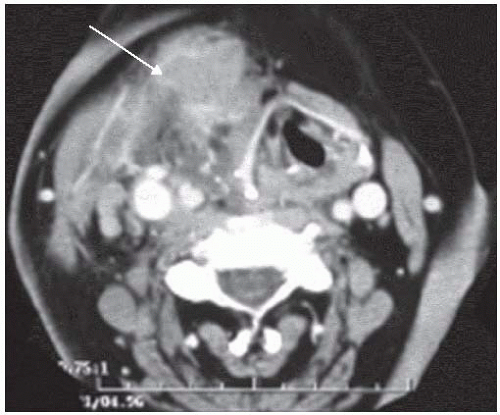 FIG 3 • CT scan of recurrent nodal disease in the lateral neck impinging upon the central compartment (arrow). CT is useful in this instance as ultrasound cannot completely define the anatomy. |
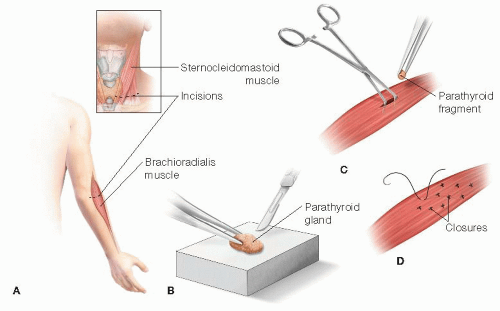 FIG 4 • Schematic of parathyroid autograft. If a parathyroid gland has been devascularized during dissection, then the best management is parathyroid autograft. A. Parathyroid glands can be grafted into any muscle; common choices include the neck muscles for normal glands and the brachioradialis muscle for abnormal glands. B. The gland should be minced into small pieces (1- to 2-mm in each dimension). C,D. The fragments are placed into individual muscle pockets. The pockets are secured with a stitch. The grafts typically require 10 to 12 weeks before measurable function.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|