Lupus Erythematosus and Variants
Julie E. Jackson, MD
Chandra N. Smart, MD
Key Facts
Terminology
Multisystem autoimmune disorder with several variants that can affect skin alone or skin and multiple internal organs
Clinical Issues
SLE: Most common systemic features are fever, weight loss, fatigue, myalgias, and lymphadenopathy
Organ systems affected include skin, joints, kidneys, hematologic, pulmonary, and central nervous
ACLE: Cutaneous form most strongly associated with systemic disease, particularly lupus nephritis
SCLE: Papulosquamous or annular erythematous rash predominantly in sun-exposed areas
Chronic cutaneous lupus erythematosus
DLE, hypertrophic LE, LE/lichen planus overlap, tumid lupus erythematosus, chilblain LE, lupus panniculitis
Lesions seen in chronic cutaneous forms of LE typically leave dyspigmentation or scarring
Microscopic Pathology
DLE
Most forms of LE have histopathologic features similar to DLE, which is thought of as the prototypic example of cutaneous lupus erythematosus
Basal layer vacuolar interface change with basement membrane thickening
Superficial and deep perivascular and periadnexal lymphohistiocytic infiltrate with increased dermal mucin deposition
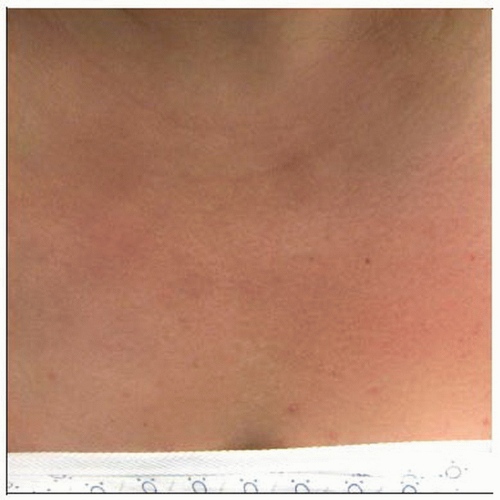 Clinical photo shows acute cutaneous lupus with photodistributed erythema (as seen on the “V” of the chest). |
TERMINOLOGY
Abbreviations
Lupus erythematosus (LE)
Definitions
Multisystem autoimmune disorder with several variants that can affect skin alone or skin and multiple internal organs
ETIOLOGY/PATHOGENESIS
Autoimmunity
Proposed complex interaction between genetically susceptible patients with an environmental or infectious agent triggering or perpetuating the immune response
Numerous genes can affect overall autoimmunity, however much focus is on genes expressing major histocompatibility complex (MHC) class II
MHC class II is an important epitope that may recognize self antigens that cross-react with infectious agents in “molecular mimicry”
Certain human leukocyte antigen (HLA) types tend to be more strongly associated
HLA-B8, HLA-DR3, HLA-DR2, HLA-A1, HLA-B15, HLA-DRw6
CLINICAL ISSUES
Epidemiology
Gender
Predominantly affects young women (20s to 30s)
F:M = 6:1
Decreases to lower ratio in purely cutaneous forms of disease but maintains female predominance
Ethnicity
Affects African-American patients more often than Caucasians
Tends to have higher mortality and higher association with systemic symptoms in African-American patients
Presentation
Systemic lupus erythematosus (SLE)
Most common systemic features are fever, weight loss, fatigue, myalgias, and lymphadenopathy
Organ systems affected include skin, joints, kidneys, hematologic, pulmonary, and central nervous as included in criteria for classification
Any form of cutaneous lupus can be associated with systemic involvement
Nonspecific cutaneous findings include
Raynaud phenomenon, periungual dilated and tortuous capillary loops, livedo reticularis, urticaria, vasculitic lesions, non-scarring diffuse alopecia
Acute cutaneous lupus erythematosus (ACLE)
Cutaneous form most strongly associated with systemic disease, particularly lupus nephritis with anti-dsDNA antibodies
Localized or generalized erythema with photosensitivity and malar rash
Subacute cutaneous lupus erythematosus (SCLE)
Papulosquamous or annular erythematous rash predominantly in sun-exposed areas that results in dyspigmentation but not typically scarring
Strongly associated with anti-Ro antibody
Neonatal lupus
Form of SCLE in neonates born to mothers with anti-Ro antibodies; typically presents as papulosquamous annular rash periorbitally and photodistributed
Neonates are also at risk for congenital heart block, hepatobiliary disease, and thrombocytopenia
Chronic cutaneous lupus erythematosus
Discoid lupus erythematosus (DLE)
Scarred, atrophic, dyspigmented plaques with follicular plugging seen typically on face, scalp, and conchal bowl
Heal with scarring, dyspigmentation, and even alopecia if scalp involvement is present
One of most common cutaneous forms of lupus with only 5-10% of patients progressing to systemic lupus erythematosus
Tends to be higher risk for progression in patients with disseminated discoid lesions
Hypertrophic lupus erythematosus
Variant of DLE with overlying thick hyperkeratotic scaling
LE/lichen planus overlap
Syndrome with clinical and histologic features of both lichen planus and lupus erythematosus that can be difficult to distinguish from lichenoid drug eruption
Can occur in lupus erythematosus patients on antimalarials
Tumid lupus erythematosus
Cutaneous form of LE with low incidence of SLE occurring as edematous plaque typically on face without overlying epidermal surface change
Chilblain lupus erythematosus
Acrally distributed dusky or purple plaques that appear or worsen in moist, cold climates
Lupus panniculitis (profundus)
Depressed, intensely scarred plaques typically on upper extremities or upper trunk occurring from involvement of panniculus
If overlying lesions of DLE are present, disease is referred to as lupus profundus
Bullous lupus
Bulla or vesicles appearing in patients with LE due to intense inflammation; can be seen in patients with ACLE, SCLE, or, rarely, DLE
Rowell syndrome
Lesions seen in acute cutaneous lupus with erythema multiforme-like lesions
Drug-induced LE
Hydralazine, procainamide, minocycline, sulfonamides, penicillin, anti-convulsants, griseofulvin (SCLE), terbinafine (SCLE), hydrochlorothiazide (SCLE), and penicillamine (unmasks true SLE)
Laboratory Tests
Serologies
ANA (95% positive in SLE), anti-double-stranded DNA (dsDNA), anti-Smith antibody (anti-Sm), antinuclear ribonucleic acid protein (rRNP), anti-La antibody
Anti-Ro antibody, anti-single-stranded DNA antibody (ssDNA), antiphospholipid antibodies (anticardiolipin antibody and lupus anticoagulant)
Systemic involvement
CBC with differential to check for anemia, thrombocytopenia, leukopenia, or lymphopenia
Serum creatinine and urinalysis for renal involvement
Other tests
Low serum complement, false-positive syphilis serologies, elevated ESR, or positive rheumatoid factor
Prognosis
Variable prognosis depending on type of LE and extent of systemic involvement, ranging from purely cutaneous disease to severe systemic disease with effect on overall morbidity and mortality
1997 Update of 1982 American College of Rheumatology Revised Criteria for Classification of SLE
For diagnosing patients in clinical studies, 4 of the following 11 criteria must be met simultaneously or serially during any time period
Malar rash
Discoid rash
Photosensitivity
Oral ulcers
Nonerosive arthritis: Involving 2 or more peripheral joints
Pleuritis or pericarditis
Renal disorder: Proteinuria > 0.5 g/day or cellular casts
Neurologic disorder: Seizures or psychosis
Hematologic disorder: Hemolytic anemia or leukopenia or lymphocytopenia or thrombocytopenia
Immunologic disorder: Positive anti DNA antibody or anti Smith antibody or antiphospholipid antibodies (anticardiolipin antibodies), lupus anticoagulant antibodies, false-positive syphilis serologic test
ANA: An abnormal titer of ANA by immunofluorescence or an equivalent assay at any point in the absence of drugs known to induce ANAs
MICROSCOPIC PATHOLOGY
Histologic Features
DLE
Hyperkeratosis with follicular dilation and keratin plugging often overlying thinned or atrophic epidermis with loss of rete ridge pattern
Basal layer vacuolar interface change over broad front with associated thickening of basement membrane that can be highlighted by periodic acid-Schiff (PAS) staining
Dermal pigmentary incontinence with dermal edema and telangiectatic vessels
Superficial and deep perivascular and periadnexal lymphohistiocytic infiltrate
Increased dermal mucin appreciated by increased clear spaces between dermal collagen bundles or spaces filled with amorphous blue material composed of hyaluronic acid
Highlighted by staining with Alcian blue or colloidal iron
Late changes include fibrosis of dermis and loss of pilosebaceous follicular units
SLE
Early lesion of malar erythema shows basal layer vacuolar change, dermal edema, and superficial and deep lymphohistiocytic infiltrate
Histology can be indistinguishable from that of SCLE and commonly DLE
Compared to DLE, thickening of basement membrane may be less with SLE
SCLE
Features classic for DLE are seen in SCLE but with more marked epidermal atrophy, less conspicuous basement membrane thickening, and less follicular plugging
Hypertrophic LE
Changes as seen in DLE with marked hyperkeratosis, hypergranulosis, and acanthosis
LE/lichen planus overlap
Histopathologic changes of both conditions are evident on biopsy
Features of lichen planus include overlying compact hyperkeratosis with wedge-shaped hypergranulosis, acanthosis, and dense lichenoid lymphocytic infiltrate leading to obscuring of dermal-epidermal junction (DEJ)
Basal layer vacuolar change with epidermal Civatte and dermal colloid bodies are also seen
Features of LE include basal layer vacuolar interface change with superficial and deep perivascular and periadnexal lymphohistiocytic infiltrate with increased dermal mucin
Tumid LE
Typically, no overlying epidermal changes are seen
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





