Lung Mass: Diagnosis
SURGICAL/CLINICAL CONSIDERATIONS
Goal of Consultation
Provide or confirm diagnosis on lung mass
If malignant, margin of specimen should be evaluated
Change in Patient Management
If diagnosis of malignancy is made, additional surgery may be performed to achieve tumor-free margins &/or stage tumor
Clinical Setting
Small masses (< 1 cm) are frequently detected by imaging
Excision is often necessary for diagnosis
˜ 70% are primary lung malignancies
˜ 10% are metastases to lung
˜ 20% are nonmalignant lesions
Large masses (> 2 cm) are generally diagnosed prior to surgery through transbronchial or CT-guided biopsy and do not necessarily require confirmation
Adenocarcinomas with pure lepidic pattern on biopsy will likely need to be fully evaluated on permanent section to exclude invasive component
SPECIMEN EVALUATION
Gross
Masses may be excised by wedge resection, lobectomy, or pneumonectomy
Pleural surface should be carefully inspected
Adhesions: May be associated with inflammatory changes or invasion of tumor through pleura
Puckering: Usually due to retraction by carcinoma that has invaded into, but not through, pleura
Pleural invasion is used for staging and is important prognostic factor
Lymphangitic spread: White color of pleural lymphatics indicating extensive lymphovascular invasion
Specimen is palpated to identify site of all masses and relationship to any pleural changes
Pleura will not move freely over carcinomas that have invaded into pleura
Specimen is completely serially sectioned to reveal any palpated mass and smaller &/or less firm masses
Any areas of possible pleural involvement should be preserved for later evaluation by permanent sections
Size and location of all masses are recorded
Distance of lesions to parenchymal margins and bronchial margins is recorded
Frozen Section
Representative section of mass is frozen
If lesion has “cheesy” or necrotic surface, touch preps may be indicated in lieu of frozen sections to avoid potential contamination of cryostat with infectious organism (e.g., Mycobacterium tuberculosis)
If surgical margin is nearby, 1 section may be able to demonstrate both diagnosis and margin
Cytology
Touch preps of cut surface of mass lesion may be helpful if conservation of tumor tissue for permanent section is necessary or if infectious granulomatous disease is possible
Suspicion for lymphoma generally requires fresh tissue to be sent for additional ancillary testing (e.g., flow cytometry, cytogenetics)
Presence of granulomas on touch prep from small necrotic mass suggests infectious etiology, and subsequent frozen section may not be indicated
MOST COMMON DIAGNOSES
Adenocarcinoma: Conventional/Nonlepidic Pattern
Most common diagnosis overall
Morphology (glandular vs. solid) depends heavily on degree of differentiation
Desmoplastic stroma or extensive chronic inflammatory response is often seen
Morphologic variants (e.g., papillary, micropapillary, and solid with mucin production) are occasionally seen
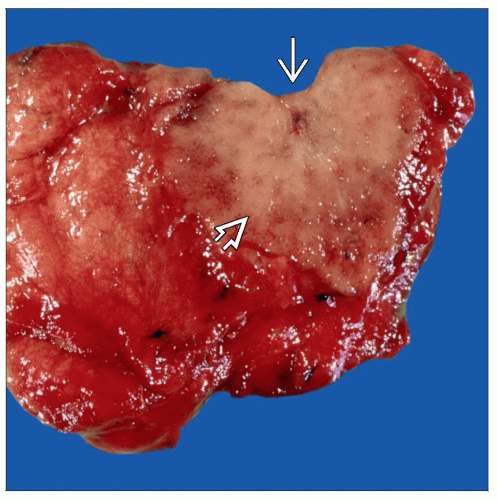
Adenocarcinoma In Situ
Synonymous term with pure lepidic pattern adenocarcinoma
Many cancers previously termed bronchioloalveolar would be in this category
By definition, mass must be < 3 cm to make this diagnosis
Often presents as ground-glass opacity on chest x-ray
Grossly forms ill-defined firmer area of lung parenchyma
Lymphomas and focal pneumonia can have similar gross appearance
This diagnosis should not be rendered without histologic evaluation of entire mass on permanent section to exclude invasion
Multiple lesions may be present
Metastatic Carcinoma/Sarcoma
Previous documented history of malignancy (e.g., colonic adenocarcinoma, osteosarcoma) is invaluable
Metastatic disease to lung is more likely to present as multiple nodules rather than as single nodule
Distinction between primary malignancy and metastasis may not always be possible at time of frozen section
Squamous Cell Carcinoma
More likely to be centrally located than adenocarcinomas
May have gritty cut surface depending on amount of keratin production by tumor
Carcinoid
Most cases occur centrally, especially in endobronchial location
Often bilobed with endobronchial component and component in bronchial wall
Patients are generally younger than typical patient with lung carcinoma
Small Cell Carcinoma
Rarely resected as many have metastasized at time of diagnosis
Non-Small Cell Carcinoma, Not Further Classified
Acceptable diagnosis in setting of poorly differentiated large cell carcinoma for which thorough sampling &/or immunohistochemistry is necessary for precise classification
Chondroid Hamartoma
Generally small and well circumscribed
Typically demonstrates blue-gray glassy cut surface due to cartilaginous composition
Granuloma
Usually small (< 1 cm) and round; may be multiple
Cut surface varies from soft/necrotic to solid/firm to bony/rock hard
Granulomas with necrotic/“cheesy” cut surface are more likely to contain fungi (e.g., Histoplasma) or mycobacteria, among other organisms
Tissue should be kept sterile and sent for cultures
Frozen sections should be avoided to minimize exposure of personnel to infectious agents and contamination of cryostat
Other Nonneoplastic Inflammatory Changes
Entities known to present with nodularities include abscess, organizing pneumonia (round pneumonia), granulomatosis with polyangiitis (Wegener granulomatosis), and hypersensitivity pneumonitis
Atypical Adenomatous Hyperplasia
Incidental finding that should not create grossly identifiable mass lesion
Size: < 5 mm in diameter
Lymphoma
Most common are extranodal marginal zone lymphoma (lymphoma of mucosa-associated lymphoid tissue) and diffuse large B-cell lymphoma
Tissue should be taken for special studies (e.g., special fixatives, frozen tissue, tissue for flow cytometry)
Intraparenchymal Lymph Node
Often located near pleura and grossly black due to anthracotic pigment
REPORTING
Frozen Section
Diagnosis of malignant or benign lesion is usually sufficient for intraoperative management
Subtypes of carcinoma are not critical intraoperatively
If patient has known primary carcinoma elsewhere, surgeon may want opinion as to whether lesion is likely metastasis or primary carcinoma
Distinction may not be possible on frozen section
PITFALLS
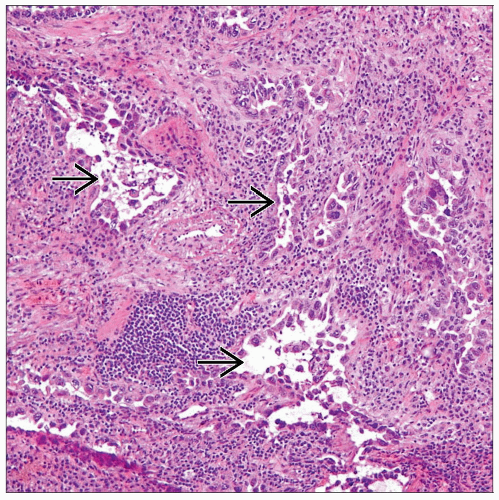
Lepidic Pattern Adenocarcinoma vs. Nonneoplastic Inflammatory Changes
Primary distinction is by the more pronounced nuclear atypia in adenocarcinomas
Adenocarcinoma is more likely to show nuclear inclusions
Carcinomas generally have thicker septal walls
Metastatic Carcinoma vs. Primary Lung Carcinoma
Important to know history of any prior malignant tumors and histologic type
May not be possible to make this distinction on frozen section
Lymphoma vs. Intraparenchymal Lymph Node
Lymphoma generally is larger with irregular border and lacks tan, fleshy cut surface of lymph node
Histologic architectural hallmarks of lymph node (capsule, subcapsular sinus, etc.) should be sought if tissue is frozen
Pure cytologic evaluation (i.e., touch prep only) may be of limited use depending on grade of lymphoma
Necrotic Malignancy vs. Necrotic Granuloma
Distinction can be challenging if lesion is totally necrotic
Malignancies (both primary and metastatic) are generally larger than infectious lesions
Granuloma formation on touch prep or frozen section suggests infectious origin, but rare exceptions exist
Tissue should be taken for cultures if infectious process is suspected
RELATED REFERENCES
1. Xu X et al: The accuracy of frozen section diagnosis of pulmonary nodules: evaluation of inflation method during intraoperative pathology consultation with cryosection. J Thorac Oncol. 5(1):39-44, 2010
2. Gupta R et al: What can we learn from the errors in the frozen section diagnosis of pulmonary carcinoid tumors? An evidence-based approach. Hum Pathol. 40(1):1-9, 2009
3. Herbst J et al: Evidence-based criteria to help distinguish metastatic breast cancer from primary lung adenocarcinoma on thoracic frozen section. Am J Clin Pathol. 131(1):122-8, 2009
4. Gupta R et al: Lessons learned from mistakes and deferrals in the frozen section diagnosis of bronchioloalveolar carcinoma and well-differentiated pulmonary adenocarcinoma: an evidence-based pathology approach. Am J Clin Pathol. 130(1):11-20; quiz 146, 2008
5. Myung JK et al: A simple inflation method for frozen section diagnosis of minute precancerous lesions of the lung. Lung Cancer. 59(2):198-202, 2008
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree