Lung: Margins
SURGICAL/CLINICAL CONSIDERATIONS
Goal of Consultation
Determine if malignancy is present at margin
Bronchial margin: Lobectomy or pneumonectomy
Parenchymal margin: Wedge resection and possibly lobectomy
Chest wall margin: For cases in which carcinoma invades from lung into chest wall
Many patients will have received preoperative therapy
Change in Patient Management
Additional tissue may be resected to achieve tumor-free margin
Results may allow further intraoperative staging of patient
Residual carcinoma at margins may be poor prognostic factor
Clinical Setting
Patient has previously diagnosed lung tumor
Complete resection with negative margins may be curative in some patients
Residual tumor at bronchial margin may compromise anastomosis
Some patients may benefit from debulking
SPECIMEN EVALUATION
Gross
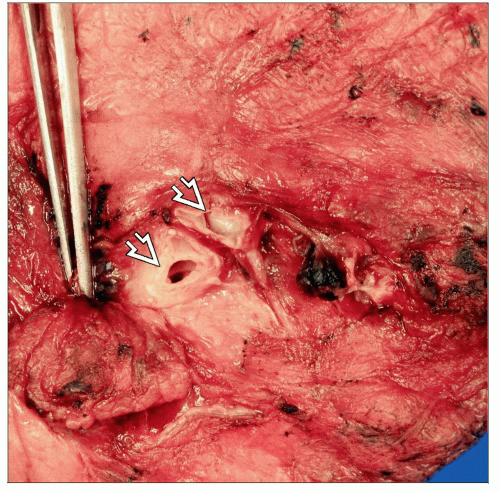
Bronchial margin
Identify bronchus protruding from specimen
Determine and record distance from tumor to margin
Adenocarcinomas can extend 2 cm to margin
Squamous cell carcinomas can extend 1.5 cm to margin
Carcinomas > 3 cm away are rarely present at margin
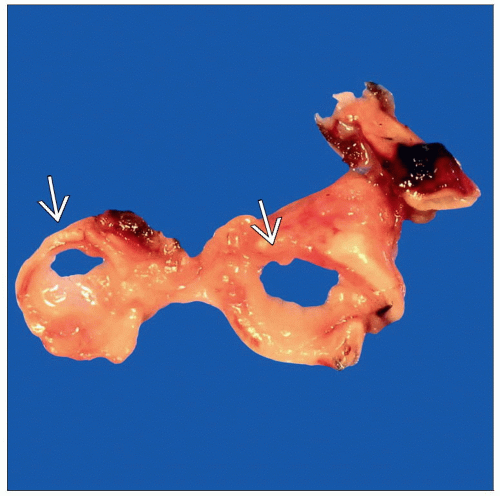
Parenchymal margin
Trim staple line as close as possible to staples
It is not practical to remove staples to examine tissue
Ink lung parenchyma revealed by opening of staple line
Chest wall margin
Identify and ink true soft tissue margin(s)
Frozen Section
Bronchial margin
En face (shave) section of entire (circumferential) bronchial ring is taken
If > 1 bronchus is present, sample all bronchi
If large, bronchial ring may be bisected &/or > 1 frozen section block prepared
Avoid including adjacent lung parenchyma and peribronchial lymph nodes
Embed with true margin face up such that true margin is 1st frozen section
Parenchymal margin
Take perpendicular section at site closest to tumor
Chest wall margin
Take perpendicular section at site closest to tumor
Transected ribs cannot be evaluated by frozen section and must be decalcified and evaluated on permanent section
Cytology
Touch preps are usually not performed on lung margins
General cytologic features of benign and malignant cells apply
Not recommended for bronchial margins as location of tumor cannot be determined
MOST COMMON DIAGNOSES
Negative for Carcinoma
By far the most common diagnosis in bronchial and lung margins
> 95% of bronchial margins are free of carcinoma
Parenchymal margins are almost never positive if lung tumor is palpable
Positive for Carcinoma
Carcinomas of salivary-like gland origin (e.g., adenoid cystic carcinoma, mucoepidermoid carcinoma) are uncommon but have higher rate of positive margins
Lymphoma may be present at margin but may not be indication for additional surgery unless there is extensive involvement and anastomosis may be compromised
Squamous cell carcinoma or small cell carcinoma is rarely at bronchial margin
Positive bronchial margin is unusual in adenocarcinoma due to its typical peripheral location
Parenchymal margin may be close or positive for carcinoma if tumor is difficult to palpate
Lepidic pattern lesions are often only slightly firm, and edges are difficult to identify
Some lepidic pattern adenocarcinomas are multifocal
Positive for Carcinoid Tumor
Endobronchial location is common site
These tumors are vascular and may be bloody upon sectioning
Carcinoma in Lymphatics
Tumor in lymphatics is generally not indication for additional surgery
It is always important to document that stromal invasion is not present
Squamous Cell Carcinoma In Situ of Bronchus
In situ carcinoma may not be indication for resection
However, stromal invasion must be excluded as this would be reason for resecting additional bronchus
REPORTING
Frozen Section
Bronchial margin
If tumor is present, report its specific location
Carcinoma in situ in bronchial mucosa
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree