Lumpectomy for Breast Cancer
Michael S. Sabel
DEFINITION
Lumpectomy is defined as the complete excision of a breast tumor with an adequate margin of surrounding normal tissue. Lumpectomy plus breast irradiation are the essential components of successful breast conservation therapy (BCT). Lumpectomies for nonpalpable cancers require wire localization. Other terms for lumpectomy include partial mastectomy, tumorectomy, or tylectomy.
PATIENT HISTORY AND PHYSICAL FINDINGS
For BCT to be successful, it must be possible to (1) obtain negative surgical margins around the tumor while still maintaining a cosmetically acceptable result and (2) safely deliver radiation therapy. A thorough history and physical examination is necessary to carefully select patients for BCT. Absolute contraindications to BCT are listed in Table 1.
A thorough history should be performed prior to treatment, including a detailed past medical history, present medications and allergies, and a personal and family history of cancer.
Prior radiation to the breast is a contraindication to BCT. For patients who may have had chest wall radiation for indications other than a prior breast cancer (such as mantle radiation for Hodgkin disease), it may be helpful to obtain the prior records and review the fields treated. These patients may be eligible for a partial breast irradiation technique (Part 5, Chapter 7).
Patients with a history of autoimmune or collagen-vascular diseases, such as scleroderma, lupus, or dermatomyositis, may have abnormal reaction to radiation therapy, which significantly compromises the cosmetic outcome. For some types of collagen-vascular disease, such as Raynaud phenomenon, rheumatoid arthritis, or Sjögren’s syndrome, the response to radiation is not as severe and these patients may be considered for BCT.
A detailed family history is critical to assess the risk of a future breast cancer, and consider genetic counseling and testing. High-risk patients may want to consider bilateral mastectomy as they are at considerable risk of a second primary cancer. The data is mixed regarding the local recurrence rate among patients with a known or suspected BRCA 1 or 2 mutations who opt for BCT. Some, but not all, studies suggest an increased risk.1,2 The decision to pursue BCT in known BRCA1/2 carriers should be made following extensive discussion with a genetic counselor.
Table 1: Absolute Contraindications to Breast Conserving Surgery
Unable to receive radiation therapy
Previous chest wall irradiation
Need to deliver radiation during pregnancy
Scleroderma or active systemic lupus erythematosus
Multicentric disease
Diffuse suspicious calcifications on mammography
Inability to achieve adequately negative margins
Patient age, nodal status, histologic tumor type, tumor grade, and extensive intraductal component (EIC) are not contraindications to BCT as long as negative margins can be obtained.
If an adequate lumpectomy can be performed, prior breast augmentation with breast implants are not an absolute contraindication, and radiation can be delivered to the augmented breast using standard techniques and doses. However, capsular contraction is a risk. If the tumor is close to the implant, preventing negative margins (cancers sometimes invade the fibrous capsule around the implant), the implant may need to be removed.
A complete, bilateral breast examination should focus on both assessing the cosmetic implications of lumpectomy and identifying additional areas of concern to rule out multicentric disease. Any additional suspicious masses should be biopsied, and cancer ruled out, prior to proceeding with BCT.
The size of the mass relative to the size of the breast, location of the mass, proximity to the skin and amount of skin needed to be resected, and symmetry of the breasts should be noted. For some patients with a large tumor relative to the size of the breast, neoadjuvant chemotherapy may be considered to downstage the primary tumor. For other patients in whom a poor cosmetic outcome with standard lumpectomy is predicted, an oncoplastic approach should be considered (Part 5, Chapter 6).
A detailed examination of the bilateral axillary, supraclavicular, and cervical lymph nodes should be undertaken, and any suspicious lymphadenopathy worked up prior to surgery.
IMAGING AND OTHER DIAGNOSTIC STUDIES
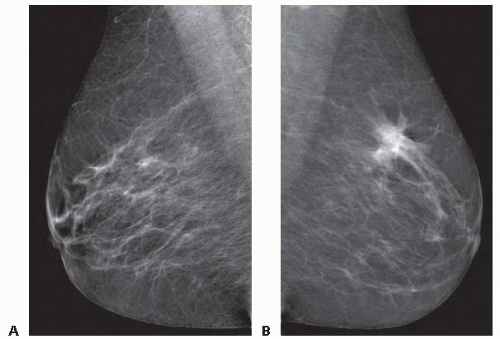
All patients require bilateral mammographic evaluation, with appropriate magnification views, within 3 months of surgery (FIG 1). The tumor size, the presence of microcalcifications, and the extent of calcifications outside of the mass should be noted. Some patients with palpable cancers may still require wire localization of the calcifications to assure complete removal at the time of lumpectomy.
Any additional areas of abnormality should be worked up and biopsied to rule out multicentric cancer. Multicentric disease is typically a contraindication to BCT; however, patients with two tumors close enough that they can be removed in one specimen with an acceptable cosmetic outcome can still be considered candidates for BCT.
The use of magnetic resonance imaging (MRI) to determine eligibility for BCT has been increasing. Although MRI may more accurately determine the extent of the tumor or identify multicentricity, particularly in women with dense breast tissue (for whom mammography is less sensitive), its use is
controversial. MRI is highly sensitive but has limited specificity and is limited in its ability to visualize ductal carcinoma in situ (DCIS). Studies have shown that the use of MRI appears to increase the mastectomy rate without decreasing reexcision or local recurrence rates.3 The need for MRI should be evaluated on a case-by-case basis.
Accurate histologic assessment of the primary tumor, including histologic subtype and hormone receptor status, is necessary in evaluating the breast cancer patient for suitability for BCT. This is best accomplished through a core needle biopsy rather than fine needle aspiration biopsy or excisional biopsy.
SURGICAL MANAGEMENT
Preoperative Planning
Prior to taking the patient back to the operating room, the presence of the palpable cancer should be confirmed with the patient. In the preoperative area, the mass should be examined in both the upright and supine positions.
With the patient in the supine position, the mass should be carefully marked.
Although the risk of infection after breast cancer surgery is low, it tends to be higher than average for a clean surgical procedure, and several studies have shown that antibiotic prophylaxis significantly reduces the risk of postoperative infection.4
Positioning
Lumpectomy is often performed in conjunction with a sentinel lymph node biopsy. Therefore, the patient should be positioned supine with the ipsilateral arm at 90 degrees.
If intraoperative analysis of the sentinel lymph node and possible axillary lymph node dissection is planned, the ipsilateral arm should be prepped into the sterile field. Otherwise, the ipsilateral arm can be secured.
If sentinel lymph node biopsy is to be performed in conjunction with lumpectomy, then the blue dye should be injected at this point. The skin is prepped with alcohol and either isosulfan or methylene blue dye is injected peritumoral (see Part 5, Chapter 8, Sentinel Lymph Node Biopsy for Breast Cancer) (FIG 2).
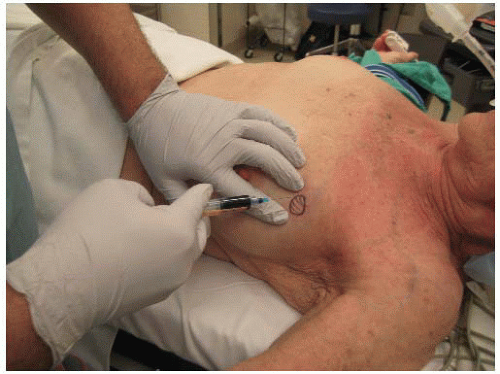 FIG 2 • Peritumoral injection of blue dye prior to lumpectomy for performance of sentinel lymph node (SLN) biopsy. |
TECHNIQUES
PLACEMENT OF INCISION
The skin incision should be placed directly over the palpable mass (FIG 3). One should avoid excessive tunneling. This may compromise the margins and make a reexcision for close or positive margins unnecessarily difficult.
When there is adequate distance between the skin and the tumor, skin does not need to be removed. However, when the tumor is close to the skin, an ellipse of skin over the tumor should be removed with the lumpectomy specimen.
In the upper hemisphere of the breast, curvilinear incisions following the Langer lines (the normal lines of tension in the skin) are ideal. In the lower hemisphere, the incisions can either be circumareolar or radial (FIG 4). For smaller tumors in relatively larger breasts, where there is adequate breast parenchyma, curvilinear incisions are acceptable. However, when skin or a fair amount of tissue is to be removed, curvilinear incisions will collapse the breast inferiorly so that the nipple points downward. In this situation, radial incisions will result in less distortion of the nipple-areolar complex.
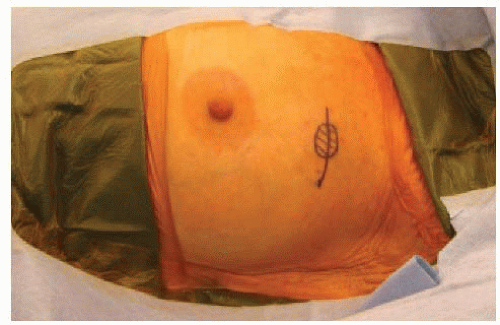
FIG 3 • Placement of incision within the Langer lines of the breast directly over the palpable cancer. The incision is planned large enough to remove the cancer without excess manipulation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access