Loop Ileostomy and Closure of Loop Ileostomy
Jennifer Hrabe
John C. Byrn
Loop ileostomy is performed whenever fecal diversion is indicated. It is often done in conjunction with other abdominal or perineal procedures. Loop ileostomy affords a technically reliable form of complete fecal diversion that is well tolerated by the patient when constructed properly. Often criticized for the risk of dehydration and small bowel obstruction, its ease of closure, low rate of infection, and reduced risk of prolapse more than correct for these concerns. This form of proximal diversion is commonly indicated for high-risk anastomoses (such as with restorative proctectomy), hostile abdomen (e.g., obstruction, sepsis, or radiation enteritis), functional colonic constipation, and temporary management of colonic or perianal inflammatory bowel disease.
SCORE™, the Surgical Council on Resident Education, classified ileostomy and closure of ileostomy as “ESSENTIAL COMMON” procedures.
STEPS IN PROCEDURE
Loop Ileostomy
Mark location preoperatively
Lower Midline Laparotomy
Identify suitable loop of ileum
Create stoma aperture with a rectus-splitting technique
Exteriorize loop of ileum
Mature stoma
HALLMARK ANATOMIC COMPLICATIONS
Loop Ileostomy
Small bowel obstruction
Dehydration
Stomal necrosis or retraction
Closure of Loop Ileostomy
Small bowel obstruction
Anastomotic leak
LIST OF STRUCTURES
Rectus abdominis muscle
Rectus sheath
Terminal ileum and cecum
Loop Ileostomy
Preparation of Ileostomy Site and Ileal Loop (Fig. 92.1)
Technical Points
The patient’s abdomen should be marked prior to surgery by either the surgeon or a trained stoma therapist. The location should avoid previous incisions, bony prominences, and skin creases. The ideal site is the right lower quadrant over the rectus muscle, but must be visible to the patient. If preoperative marking is not possible, consider placing the ostomy high on the right side of the abdomen where there will be fewer skin creases and the patient will be able to see and care for it appropriately. The stomal incision should be appropriately spaced from the midline incision; too close will make pouching difficult, whereas a more lateral incision is likely to lie outside of the rectus muscle.
The patient should be positioned supine. If the abdomen is not already open, make a short vertical midline incision. Select the most distal ileal segment that reaches the desired site on the abdominal wall without tension. If necessary, mobilize the terminal ileum by incising any lateral peritoneal attachments. Avoid excess mobilization, however, as an overly mobile ileum may be at greater risk for volvulus. Using a hemostat, make a window in the mesentery adjacent to the portion of ileum that will be used for the stoma. Pass a Penrose drain through this defect and clamp the drain. The Penrose drain will provide atraumatic manipulation of the bowel through the abdominal wall. Mark the bowel with two seromuscular sutures to ensure maturation of the
correct limb. Place a blue vicryl suture proximally and a brown chromic suture distally.
correct limb. Place a blue vicryl suture proximally and a brown chromic suture distally.
Before incising the stoma site skin, place one Kocher clamp on the midline incision fascia and one on the overlying dermis. These will keep the layers of the abdominal wall aligned during stoma creation. Hold the clamps in the palm of your nondominant hand and, with a laparotomy pad to protect intra-abdominal contents, elevate the abdominal wall with your fingers. Excise a 2-cm disc of skin at the marked ostomy site. Incise the subcutaneous tissue vertically and use right-angle retractors to reveal the underlying anterior rectus abdominis fascia. Make a 2-cm vertical incision in this fascia. Gently separate the rectus abdominis muscle fibers with a curved blunt instrument, then use right-angle retractors to retract the muscle and reveal the posterior rectus fascia. Incise the posterior fascia and underlying peritoneum. Check the opening diameter. It should be approximately two fingers’ breadth.
To detect occult injuries to the inferior epigastric artery, pass a dry sponge through the stoma track. Clamp the ends of the sponge with a Peon and complete any remaining intra-abdominal portions of the procedure.
Anatomic Points
The rectus abdominis is significantly wider superiorly than inferiorly, transitioning from a broad, thin muscle to a narrow, thick one. Above the arcuate line, it is enclosed by the rectus sheath, which is formed from the aponeuroses of the external and internal oblique and the transversus abdominis muscles. Ostomies located outside of the rectus sheath have been associated with higher rates of parastomal hernias.
Most of the ileum lies in the right lower quadrant. It is approximately 2 to 3 cm in diameter and several meters long. It is attached to the posterior abdominal wall by the mesentery. The terminal ileum is typically in the pelvis and then ascends to the medial portion of the cecum. A fold of peritoneum, the ileocecal fold, connects the antimesenteric terminal ileum to the cecum and vermiform appendix. The ileal blood supply is the superior mesenteric artery (SMA) which gives off arterial arcades that lead to the vasa recta. The terminal ileum is supplied by the ileal branch of the ileocolic artery. Venous drainage is via the superior mesenteric vein and mirrors the SMA.
Creating the abdominal defect of the stoma requires one to traverse all layers of the abdominal wall. Beneath the skin is the variably thick layer of Camper’s fascia. Superior to the arcuate line, the rectus muscles are covered both anteriorly and posteriorly by the aponeuroses of the lateral abdominal wall muscles. The arcuate line position varies between individuals, but generally is one-third the distance from the umbilicus to the pubic symphysis. Inferior to the arcuate line, the rectus sheath covers only the anterior surface of the rectus abdominis muscles. Deep to the rectus sheath is the transversalis fascia and then the parietal peritoneum. It is this transversalis fascia that should be kept aligned with the overlying tissues to ensure alignment of
ostomy defects. The inferior epigastric artery runs superiorly in the transversalis fascia and enters the rectus sheath inferior to the arcuate line. It runs posterior to the rectus abdominis, and near the umbilicus, anastomoses with branches from the superior epigastric artery.
ostomy defects. The inferior epigastric artery runs superiorly in the transversalis fascia and enters the rectus sheath inferior to the arcuate line. It runs posterior to the rectus abdominis, and near the umbilicus, anastomoses with branches from the superior epigastric artery.
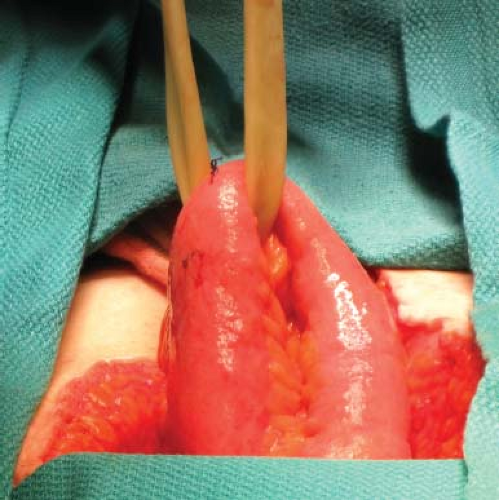 Figure 92.2 Loop of ileum is exteriorized. Note the Penrose drain used for gentle retraction, and the blue stitch (proximal) and brown chromic stitch (distal) to assure accurate orientation.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
