Lobectomy
Phillip C. Camp
M. Victoria Gerken
Pulmonary lobectomies are most commonly performed for carcinoma. Resection of a more limited amount of pulmonary tissue allows preservation of the maximum amount of lung function. Even more limited segmental and subsegmental resections are possible and are described in the references at the end.
Steps in Procedure
Single-lung ventilation, lateral decubitus position, posterolateral thoracotomy
Right Upper Lobectomy
Retract lung inferiorly and posteriorly
Incise pleura around the hilum
Identify superior pulmonary vein and dissect distally, preserving middle lobe vein
Isolate pulmonary artery and similarly dissect
Retract lung anteriorly and incise pleura overlying bifurcation of upper lobe bronchus and bronchus intermedius
Divide superior arterial trunk, followed by superior pulmonary vein
Divide the distal pulmonary artery and complete the division of the fissure, if necessary
Retract lung anteriorly and divide branches of vagus nerve to upper lobe
Divide bronchus with linear stapler, 4.8 cartridge
Finally, divide the posterior ascending pulmonary artery branch
Divide any remaining attachments
Incise inferior pulmonary ligaments to allow remaining lung to move cephalad
Check hemostasis and check for air leaks
Close thoracotomy incision with chest tubes
Right Middle Lobectomy
Initiate dissection at confluence of major and minor fissure
Identify middle lobe branch of pulmonary artery and divide it
Retract lung posteriorly and divide mediastinal pleura
Dissect and divide branches of superior pulmonary vein draining middle lobe
Place stapler across bronchus and close it
Before firing, confirm that basal segments of remaining lung still inflate
Divide bronchus
Proceed with closure as noted above
Right Lower Lobectomy
Start the dissection at the confluence of fissures
Identify pulmonary artery
Open the pleura over the interlobular artery
Mobilize the pulmonary artery
Ligate and divide the superior and then the basilar segmental branches separately
Divide inferior pulmonary ligament and incise pleura over the inferior pulmonary vein and bronchus intermedius
Mobilize and divide inferior pulmonary vein at pericardial reflection
Open posterior mediastinal pleura and divide bronchus
If necessary, complete fissure with stapler
Left Upper Lobectomy
Retract lung inferiorly, open pleura over superior hilum
Expose left main pulmonary artery and obtain proximal control
Incise pleura over medial aspect of the superior pulmonary vein
Complete the fissure if necessary
Dissect and divide branches of the pulmonary artery, followed by pulmonary vein
Divide the bronchus
Divide inferior pulmonary ligament to allow the remaining lung to fill the pleural space
Left Lower Lobectomy
Retract lung anteriorly and incise pleura from bronchus to level of inferior pulmonary ligament
Divide inferior pulmonary ligament to level of inferior pulmonary vein
Complete fissure if necessary
Dissect pulmonary artery and ligate branches to lower lobe
Similarly divide branches of pulmonary vein
Apply stapler across bronchus, check remaining lung for inflation
Fire stapler
Hallmark Anatomic Complications
Bronchial stump leak
Injury to pulmonary artery or vein
Impingement on adjacent bronchus during bronchial division, resulting in segment of lung that is not aerated
List of Structures
Right Main Pulmonary Artery
Superior branch
Posterior segmental artery
Right Superior Pulmonary Vein
Branches to anterior and apical segments
Posterior segmental vein
Right inferior pulmonary vein
Right upper lobe bronchus
Intermediate Bronchus
Middle lobe bronchus
Right lower lobe bronchus
Major fissure
Minor fissure
Middle lobe
Inferior pulmonary ligament
Left Pulmonary Artery
Arteries to the apicoposterior segment
Anterior segmental artery
Lingular artery
Branch to the superior segment of the lower lobe
Basilar segmental artery
Left inferior pulmonary vein
Left Superior Pulmonary Vein
Apicoposterior segmental vein
Lingular segmental veins
Anterior basal segmental vein
Left Lower Lobe Bronchus
Left upper lobe bronchus
 |
Right Upper Lobectomy
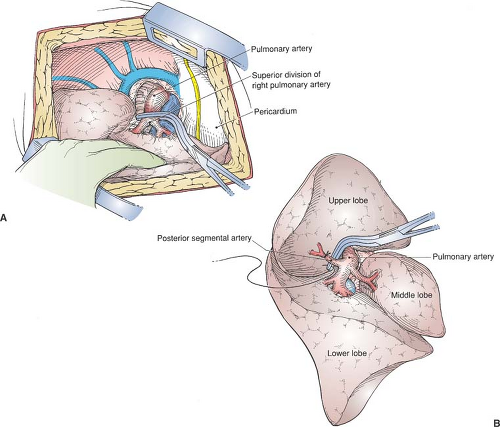
Ligation of the Pulmonary Arteries (Fig. 27.1)
Technical Points
Secure the left endobronchial double-lumen tube, allowing single-lung ventilation for the duration of the resection. Place the patient in the left lateral decubitus position and make a right posterolateral thoracotomy. A muscle-sparing thoracotomy is a feasible alternative, but should never be allowed to hinder the resection.
Retract the lung inferiorly and posteriorly and divide the pleura around the hilum.
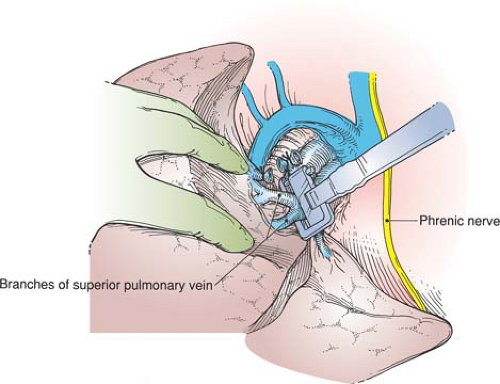
Identify the superior pulmonary vein and dissect along it distally up to the lung parenchyma. Mobilize around the vessel in the appropriate plane. Identify and preserve the middle lobe vein, which typically enters the superior pulmonary vein. Be alert to aberrant venous drainage, including occasional direct connections to the vena cava.
The pulmonary artery lies just posterior and superior to the vein (Fig. 27.1A). Gently develop the appropriate plane, and dissect proximally and distally. The pulmonary artery is an extremely delicate and unforgiving vessel. Great care and attention to detail will aid in successful mobilization. Mobilize circumferentially and place an umbilical tape loosely around it to provide proximal control should bleeding occur.
Distal dissection will identify the truncus anterior (apicoanterior) branch. Dissection should be circumferential and should avoid spreading of surrounding tissue. Gently passing a blunt curved clamp can help define planes. Never pass the clamp against resistance. “Peanut” dissection is often useful for better defining the anatomy after you are in the correct plane. Free the pulmonary artery from the upper lobe branches and any attachments to the azygos vein.
Retract the lung anteriorly and incise the pleura overlying the bifurcation of the upper lobe bronchus and bronchus intermedius.
Careful use of electrocautery will control small bronchial vessels in this area. Reliably, a lymph node is located at this point and is swept anteriorly. Anterior to the lymph node is the superior segment branch of the pulmonary artery to the lower lobe, which is much better seen from this aspect than by the anterior approach. After you have identified this branch, any intact portion of the posterior aspect of the major fissure can be completed (divided) with staplers. This posterior approach to the superior segment branch greatly improves the anatomic division and is rather efficient (Fig. 27.1B).
Careful use of electrocautery will control small bronchial vessels in this area. Reliably, a lymph node is located at this point and is swept anteriorly. Anterior to the lymph node is the superior segment branch of the pulmonary artery to the lower lobe, which is much better seen from this aspect than by the anterior approach. After you have identified this branch, any intact portion of the posterior aspect of the major fissure can be completed (divided) with staplers. This posterior approach to the superior segment branch greatly improves the anatomic division and is rather efficient (Fig. 27.1B).
Divide the apical segmental vein, crossing the anterior segmental artery, either with vascular staples or with suture ligatures.
Mobilize and divide the superior arterial trunk with a vascular stapler or suture ligature. Ligate apical and segmental branches.
Anatomic Points
Remember that the azygos vein arches from posterior to anterior immediately superior to the root of the right lung, and that, at least conceptually, the plane of the major pulmonary veins is anterior to that of the arteries. The right pulmonary artery, at the point where it leaves the pericardial sac, is anterior and somewhat inferior to the right main-stem bronchus. It enters the minor fissure and passes inferolaterally anterior to the upper lobe bronchus. Slightly before it enters the minor fissure, it gives off a superior branch from its superior aspect, which can supply all three segments of the upper lobe. Frequently, however, the superior trunk supplies only the apical and anterior segments, whereas the posterior segment is supplied by an ascending artery that branches off the superior aspect of the main pulmonary artery, somewhat distal to the superior branch.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree