Liver: Evaluation of Allograft Prior to Transplantation
SURGICAL/CLINICAL CONSIDERATIONS
Goal of Consultation
Evaluation of a donor liver prior to transplantation
Change in Patient Management
Pathologic findings are used to decide whether or not liver is suitable for transplantation
Unlike kidney transplantation, there is no alternative should the allograft fail
Livers with a high risk of allograft failure will not be used for transplantation
Clinical Setting
There is a shortage of donor livers available for transplantation
Criteria for acceptance have been expanded to include organs at a greater risk of reduced function or graft failure
The following features are no longer used to exclude a liver from consideration
Age (> 60 years), viral hepatitis, steatosis, alcohol abuse, acute infection, hypotension, hypoxemia, cardiovascular disease, chronic renal failure
Histologic evaluation of liver is helpful to predict organs at greatest risk
Degree of macrovesicular steatosis is most useful criteria for accepting or rejecting a graft
SPECIMEN EVALUATION
Gross
Either a wedge biopsy (≥ 1.5 cm²) or a cutting needle biopsy (≥ 2 cm in length) from anterior-inferior edge of kidney is performed
If a gross mass lesion is present, separate biopsy of noninvolved liver also should be evaluated
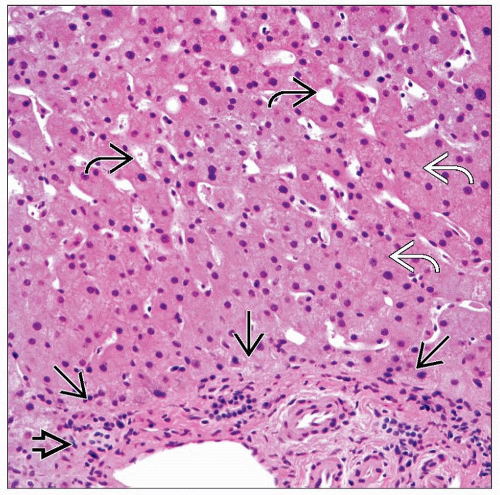
Needle biopsy is preferred for evaluating fibrosis
Subcapsular liver sampled in wedge biopsy often has thick trabeculae that may be mistaken for advanced fibrosis
Biopsy should be processed as quickly as possible
Fat is diminished after even a few minutes of exposure to air
Saline can cause distortion (chromatin clumping and edema of extracellular spaces)
Frozen Section
Tissue should be gently blotted dry to reduce ice crystal artifact
Representative slides should be retained by recipient institution to aid in evaluating graft after transplantation
FEATURES TO BE EVALUATED
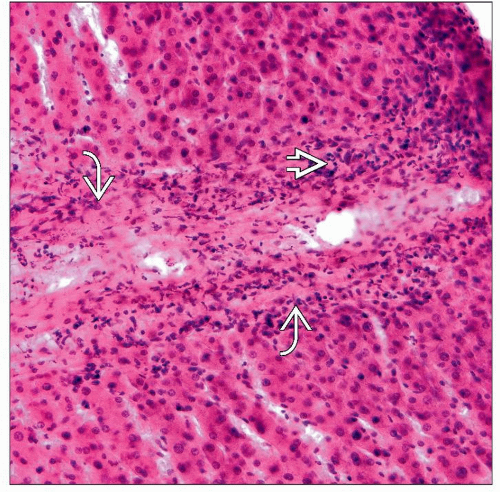
Macrovesicular Steatosis
Single, dominant, lipid vacuole displacing nucleus to periphery of cell
Usually centrilobular
Severity is graded
Mild: < 30% of hepatocytes
Moderate: 30-60% of hepatocytes
Increased risk of complications
Liver may be accepted for transplant in some settings
Severe: > 60% of hepatocytes
Absolute contraindication for transplantation due to high risk of graft malfunction
Microvesicular Steatosis
Numerous small lipid droplets that do not cause displacement of nucleus to periphery of cell
Nucleus is located in center of cell
Graded in same manner as macrovesicular steatosis
Minimal effect on graft function
Common finding
Fibrosis
Necrosis
Apoptotic hepatocytes (acidophil bodies)
Centrilobular necrosis
Reported as
Focal (< 10%) or extensive (≥ 10%)
Mild or severe
Mass Lesions
Benign lesions are not a contraindication for transplantation
Biopsy away from mass should also be evaluated
Carcinoma
Detection of tumor cells is absolute contraindication for transplantation
Portal Inflammation
Mild chronic inflammation of portal triad is common in hospitalized patients; not a contraindication
Severe lymphoplasmacytic portal infiltrate with interface hepatitis (piecemeal necrosis) should raise possibility of viral hepatitis
Reported as mild, moderate/severe
Iron Deposition
Hepatocellular siderosis
Coarse, dark brown granular pigment in periportal hepatocytes; graded semiquantitatively 1-4+
Grades > 2 may be contraindication for transplantation
Organs from patients with hereditary hemochromatosis or secondary iron overload can be used if fibrosis is not advanced
Kupffer cell siderosis
Common finding; typically mild, cannot be detected easily on frozen section
Other Pigments
Lipofuscin (very fine brown granules in centrilobular hepatocytes)
Bile (green to gold/brown granules) in perivenular hepatocytes or within canaliculi
Granulomas
Nonnecrotizing fibrotic granulomas may be residue of prior infection (e.g., histoplasmosis); not contraindication to transplant
Necrotizing granulomas may indicate current infection and lead to rejection of organ for transplant
Congestion
Dilated sinusoids alone are a nonspecific finding
Atrophy of perivenular hepatocytes and sinusoidal dilatation often consequence of terminal ischemic injury
Duct Damage
Seen in primary biliary disorders, such as primary biliary cirrhosis and primary sclerosing cholangitis
Ductular proliferation is also indirect evidence of duct damage
Thrombi
Rarely seen in central or portal veins
REPORTING
Frozen Section
Features reported
Steatosis: Presence or absence and percent of hepatocytes affected
Minimal or mild (up to 30% of hepatocytes) may be acceptable for transplantation
Severe (> 60%) is associated with a nonfunctioning graft
Extent of inflammation &/or hepatocyte necrosis
Mild focal necrosis may occur during harvesting of organ
Severe or extensive necrosis is associated with graft failure
Fibrosis: Presence or absence
Alcohol-induced injury: Associated with compromise of graft weeks to years after transplantation
Fibrosis
Moderate to severe fatty change
Marked hepatocytic necrosis with or without cholestasis
Mallory hyaline/ballooning degeneration
Biopsies consisting entirely or predominantly of capsule are inadequate for evaluation
Additional biopsy should be requested
PITFALLS
Superficial Biopsy
Very superficial biopsy may only sample the capsule
Glisson capsule can penetrate into parenchyma for 0.5 cm or more
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree