Left Colectomy for Colon Cancer
Saul J. Rugeles
Luis Jorge Lombana
DEFINITION
Left colectomy for cancer is defined as the resection of the left colon in which the extension must correspond to the distribution of the lymphovascular drainage of the tumorcompromised segment, having as the result negative borders on histopathologic studies, along with in block extirpation of the lymphovascular tissue that nurtures that zone of the colon with a minimum number of 12 lymph nodes available to be evaluated by a histopathologic study.1
DIFFERENTIAL DIAGNOSIS
Most of patients with left colon tumors must have a cancer histologic diagnosis before being taken to surgery.
However, there are existing cases in which the biopsies taken by colonoscopy do not identify the presence of a neoplasia. In these cases, it is recommended to take another biopsy set. If a second set is not diagnostic, it is recommended to proceed with the colectomy and obtain the pathologic study from the surgical specimen.
The differential diagnoses for left colon cancer include complicated diverticular disease with stenosis, intraluminal foreign bodies with an inflammatory reaction, neoplastic invasion from adjacent organs (especially ovaries), and colonic endometriosis.
PATIENT HISTORY AND PHYSICAL FINDINGS
The patient’s medical record must be complete, including a detailed description of signs and symptoms; medical history, with special attention to the evolution of symptoms; food intake and weight changes; and a thorough physical examination, including rectal examination. The abdomen must be carefully palpated, aimed to search for lumps, carcinomatosis, or ascites. The lymphatic nodal basin must be examined as well.
Family history of cancer is especially important, including two generations, and asking for the presence of colon, gastrointestinal, breast, endometrial, and prostate cancer. This will allow the identification of possible cases of familiar colon cancer.
The clinical evaluation must include a subjective global assessment of nutritional status to identify the patients who may benefit from perioperative nutritional therapy.2
The physiologic risk of the patient must be evaluated according to his or her age, intercurrent diseases, and type of surgery, following the institutional preoperative evaluation guidelines.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Carcinoembryonic antigen (CEA): The baseline preoperative result and postsurgical control must be obtained as an assessment for complete tumor resection. On the other hand, the absolute presurgical value is an independent variable for survival.1
Abdominal computed tomography is the most sensitive and specific test for detection of intraabdominal metastases.1
Chest computed tomography is the most sensitive and specific test to detect mediastinal and lung metastases.1
Total colonoscopy: Regardless of the primary localization of the tumor, every patient should have a complete colonoscopy study whenever possible, because 2% to 9% of the patients may have synchronous tumors.1 The colonic enema with double contrast may be used in those patients in whom the colonoscopy is not possible.
Tumor histologic studies that describe the cell differentiation and the extent of the invasion.
SURGICAL MANAGEMENT
Preoperative Planning
The extension and type of procedure must be thoroughly discussed with the patient and family. This includes the possibility of a temporary or permanent colostomy.
Left colectomy is a major surgery that has potential for postoperative morbidity and mortality. It is desirable to discuss with the patient the local statistical rates for morbidity and mortality before obtaining the informed consent.
There is controversy about the effectiveness and need of mechanical preparation of the bowel before the colectomy.3, 4, 5 I personally use a “mild” preparation with 2 days of liquid diet and polyethylene laxatives the day before the surgery, achieving the evacuation of large fecal residues. I do not demand a crystalline wash before the surgery.
In the operating room, before initiating the anesthetic act, it is desirable to follow a checklist in which every professional involved in the surgical act must participate. This list should include at least patient identification, type of surgery, type of anesthesia, expected events during the surgery, the need for blood components, prophylactic antibiotic, surgical devices availability, and potential adverse events and their prevention.
Positioning
The surgery is performed with the patient in a supine position. The arms should ideally be tucked to the sides, allowing freedom of movement for the surgical team. If one extended arm is required, it should be placed at an angle of 90 degrees and the right arm is preferred.
If a colorectal anastomosis with a circular stapler is assumed, the patient should be in the lithotomy position. In this case, one must ensure that the patient’s thighs maintain a horizontal plane with the patient’s abdomen, for them not to interfere with the surgeon’s arms (FIG 1). The lower extremities’ position in the brackets must protect them from neuropraxias or vascular compressions.
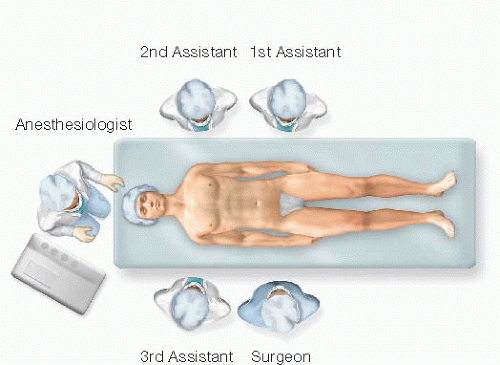
The surgical team setup is shown in FIG 2.
The surgical table must allow inclinations in every way, which will be necessary to expose regions with difficult access, such as the splenic flexure of the colon.
The patient must be secured to the surgical table adequately to prevent body displacements with position changes of the surgical table.
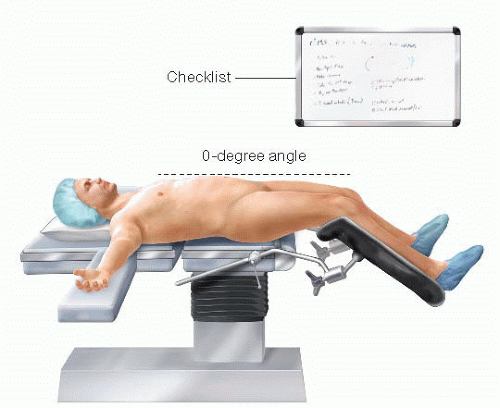 FIG 1 • Correct position of the patient in the operating table. Note the horizontal position of the thighs to ensure free movement of surgeon’s arms and hands. |
TECHNIQUES
LAPAROTOMY, REVISION OF PERITONEAL CAVITY, AND SURGICAL FIELD PREPARATION
A medial supra- and infraumbilical laparotomy is performed, carrying the incision down to the pubis, which will improve pelvic exposure. Once the abdominal cavity is opened, it is advisable to protect the wound edges from bacterial and cellular contamination by placing an Alexis® wound protector or similar instrument (FIG 3A,B).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree