Larynx: Diagnosis and Margins
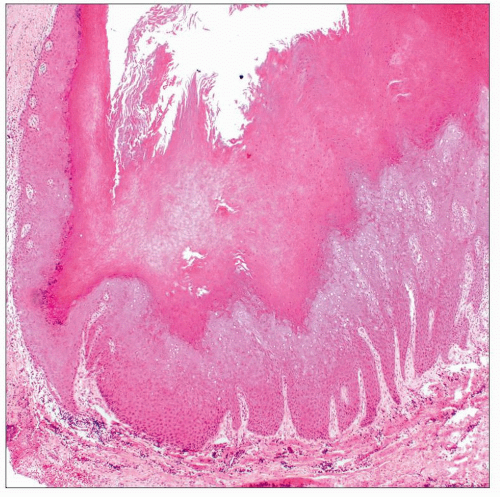
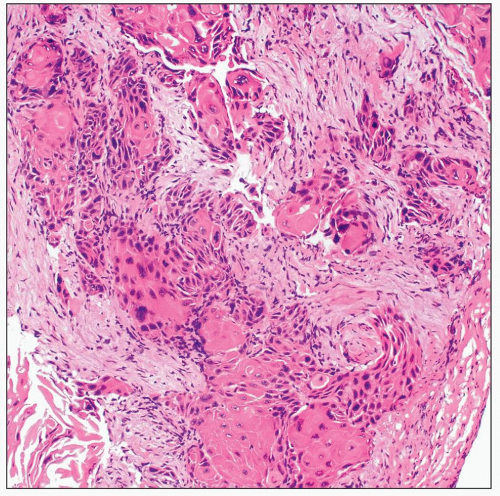 Invasive keratinizing squamous cell carcinoma is characterized by irregular nests of atypical squamous epithelium, with focal areas of keratinization, eliciting a loose desmoplastic stromal response. |
SURGICAL/CLINICAL CONSIDERATIONS
Goal of Consultation
Determine if malignancy or dysplasia is present
Determine if margins are free of carcinoma or dysplasia
Change in Patient Management
Carcinoma may be excised or treated with radiation therapy if margins positive
Multiple biopsies may be used to map extent of tumor and determine how much tissue to excise
Additional tissue may be taken at areas of margin involvement to obtain clear margins
Clinical Setting
Smoking and alcohol use are major risk factors for conventional squamous cell carcinoma
Patients with advanced carcinoma, airway compromise, or recurrent carcinoma may undergo a total laryngectomy
Patients with limited involvement or in situ carcinoma may be treated with a partial laryngectomy
SPECIMEN EVALUATION
Gross
Biopsies are often small and fragmented
Total laryngectomy
Superior mucosal margins are the margins most likely to be positive for carcinoma
Anterior/lateral soft tissue margins may be involved if tumor is advanced
Separate margins may be submitted as small specimens by surgeon
Specimen may contain additional pharyngeal or thyroid tissue
Partial laryngectomy
Orientation by surgeon may be necessary
Separate margins may be submitted as small specimens by surgeon
Frozen Section
Small biopsies and separate margins may be completely frozen
If mucosa can be identified, specimen should be embedded in a way to allow for vertical sections and assessment of invasion
Margins should always be taken perpendicular to actual margin
En face margins are not capable of evaluating narrow (1-2 mm) but tumor free margins
Distance to margin cannot be determined and may be clinically important
MOST COMMON DIAGNOSES
Keratinizing (Conventional) Squamous Cell Carcinoma
Tumor may exhibit differing patterns of invasion
Broad pushing front of invasion
This pattern is especially challenging in small biopsies and may require presence of adjacent normal tissue to recognize presence of invasion
Irregular nests of tumor cells &/or individual infiltrative cells
This is a more obvious pattern of invasion and can be recognized in small biopsies
Abnormal keratinization, frequent mitoses, necrosis, nuclear pleomorphism and hyperchromasia, &/or a desmoplastic stromal response may be appreciated
Verrucous Carcinoma
Extremely well-differentiated variant of squamous cell carcinoma with minimal cytologic atypia
Uniform front of invasion with bulbous rete ridges
When strictly defined, only poses risk of local recurrence
Diagnosis should be reserved for excised tumors, as similar features may be seen in areas of a conventional squamous cell carcinoma
Basaloid Squamous Cell Carcinoma
Clinically aggressive variant
Basaloid tumor cells with scant cytoplasm and high-grade features including necrosis, nuclear hyperchromasia, and frequent mitoses
Histologic recognition as squamous carcinoma relies on identification of squamous differentiation (keratinization or intercellular bridges) or a coexisting component of squamous dysplasia/carcinoma in situ
Must be distinguished from oropharyngeal human papillomavirus (HPV)-associated squamous cell carcinoma, which has a favorable prognosis
Also must consider other high-grade small round cell malignancies, especially small cell carcinoma
Distinction often requires special stains
Adequate on frozen section to diagnose as a basaloid carcinoma and defer to permanent sections
Sarcomatoid (Spindle Cell) Carcinoma
Recognized by presence of a malignant spindle cell proliferation coexisting with conventional squamous cell carcinoma &/or squamous dysplasia
Behaves similarly to conventional squamous cell carcinoma
In absence of dysplasia or carcinoma in situ, preliminary diagnosis of atypical spindle cell proliferation may need to be given
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree