Laparoscopic Roux-en-Y Gastric Bypass
James W. Maher
Laparoscopic Roux-en-Y gastric bypass, one of the most technically demanding laparoscopic procedures, is emerging as the preferred method for treating morbid obesity when nonsurgical therapy has failed.
Steps in Procedure
Obtain laparoscopic access and place patient in reversed Trendelenburg position
Assistant retracts omentum and fundus inferiorly
Excise gastroesophageal (Belsey’s) fat pad
Incision peritoneum and gently dissect behind cardial notch (angle of His)
Anesthetist inserts Baker tube into stomach, inflates balloon with 15 mL saline, and gently withdraws until resistance is felt (balloon stopped by gastroesophageal junction)
Mark distal extent of balloon on serosal surface of stomach using electrocautery
Divide lesser curvature vessels below this with ultrasonic shears
Enlarge opening and gently dissect to connect with opening on greater curvature.
Withdraw Baker tube (and any other tubes/devices within stomach)
Divide stomach at level previously marked using endoscopic linear cutting stapler
Clear any adhesions in lesser sac and insert white Penrose drain into sac
Take table out of reverse Trendelenburg position and move scope holder to patient’s left
Identify suspensory ligament of duodenum (ligament of Treitz) and create opening in mesocolon, entering lesser sac and visualizing Penrose drain
Divide jejunum 30 cm distal to suspensory ligament of duodenum (ligament of Treitz) with endoscopic linear cutting stapler
Mark distal bowel with suture to avoid confusion
Trace the jejunum for an additional 75 cm distal to point of transaction and approximate antimesenteric border of proximal bowel to antimesenteric border of this region
Anastomose with endoscopic cutting linear stapler, place additional antiobstruction suture and close mesenteric defect
Suture distal jejunum (with marking suture) to Penrose drain and use this to pass the jejunum into the lesser sac, avoiding torsion
Anastomose to gastric pouch with hand-sewn anastomosis
Close defect in mesocolon
Place closed suction drain behind gastrojejunostomy, bringing it out through a lateral trocar site
Close all trocar sites over 5 mm
Hallmark Anatomic Complications
Injury to bowel or viscera during laparoscopic access
Injury to esophagus
Injury to stomach
Confusion as to proximal or distal loop of jejunum
Loop torsed when passed through mesocolon
Postoperative herniation through defect in mesocolon
List of Structures
Umbilicus
Stomach
Fundus
Incisura
Cardial notch (angle of His)
Greater curvature
Lesser curvature
Esophagogastric junction
Esophagus
Belsey’s fat pad
Greater omentum
Lesser (gastrohepatic) omentum
Jejunum
Suspensory ligament of duodenum (ligament of Treitz)
Transverse Colon
Mesocolon
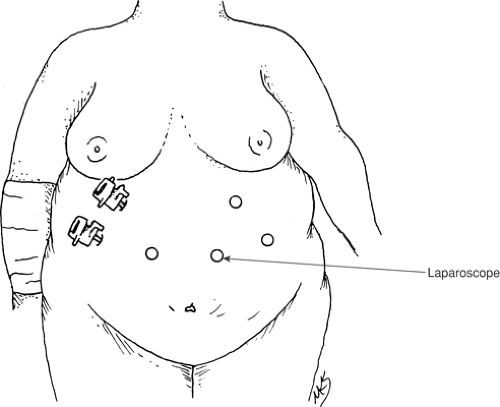
Patient Position and Trocar Position (Fig. 60.1)
Technical and Anatomic Points
A Foley catheter is inserted into the bladder. The patient is positioned supine on the table with the right arm tucked to the side. The left arm is positioned on an arm board. A foot board is applied to the end of the table to facilitate placement of the patient in reverse Trendelenburg position to aid exposure in the upper abdomen.
The surgeon stands on the patients right, the assistant and scope holder on the patients left. Elevate the umbilical plate with two Allis clamps and insert a Veress needle into the abdomen approximately 15 cm below the xiphoid and 2 to 3 cm to the left of the midline. Do not use the umbilicus as a landmark because it is displaced inferiorly in many morbidly obese patients. Insufflate the abdomen with a high flow insufflator to an intraabdominal pressure of 15 cm water. Next insert a 5-mm trocar in the left upper quadrant and place a 5-mm, 30-degree scope to guide insertion of the other trocars. The next trocar is a 5-mm trocar inserted in the right upper quadrant laterally to allow liver retraction. Insert a 10-mm trocar into the midepigastrium to the patient’s left. Its position should generally be just below the level at which the ligamentum teres begins. This trocar will be used for the 10-mm, 45-degree scope throughout the procedure. Insert a 12-mm port at the same level in the right epigastrium; this will serve as one of the surgeons’ operating ports. Take care not to place this port too inferior because this may compromise the ability of the instruments to reach the operating area. Next place the liver retractor. Retract the liver superiorly and fix the retractor to the table with a retractor holder to provide stable exposure. Insert another 5-mm trocar into the right upper quadrant as the second operating port. Take care to place this port below the liver retractor and free of the round ligament. Inserting a long needle through the abdominal wall in the proposed trocar site may help prevent misplacement of this trocar. Finally, place a fourth 5-mm trocar in the left upper quadrant as a second port for the assistant.
Exposure of the Cardial Notch (Angle of His) (Fig. 60.2)
Technical Points
Place the patient in reverse Trendelenburg position. The assistant retracts the omentum as well as the fundus inferiorly. A fat pad known as the gastroesophageal fat pad, or Belsey’s fat pad, overlies and in many cases obscures the gastroesophageal junction and the cardial notch (angle of His). Excise this pad with an ultrasonic shears to expose the cardial notch (angle of His) (Fig. 60.2A). Incise the peritoneum in this area with the ultrasonic shears and gently dissect the area behind the cardial notch (angle of His) with an articulating angled dissector (Fig. 60.2B).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree