Laparoscopic Right Hemicolectomy
Craig A. Messick
Joshua S. Hill
George J. Chang
DEFINITION
Right hemicolectomy is defined as the resection of a portion of the terminal ileum, cecum, ascending colon, and portion of the transverse colon. When performed for neoplastic disease, it includes resection of the vascular pedicles including the ileocolic, right colic (when present), and sometimes right branch of the middle colic artery and their associated veins. An extended right hemicolectomy is one in which the middle colic vessels are ligated. Laparoscopic right hemicolectomy has been shown to be a preferred alternative technique in the resection of benign and malignant diseases of the colon and in experienced hands has been shown to have equivalent oncologic outcomes with improvements in speed of recovery when compared to open resection.1, 2, 3
INDICATIONS
Right hemicolectomy may be performed for either benign or malignant indications, but the underlying principles of surgical resection apply to both open and laparoscopic approaches. A thorough preoperative workup to define the underlying disease plays a critical role in determining the nature of the operative intervention and optimizing the surgical treatment.
Benign pathology (common etiologies)
Crohn’s disease: most frequently occurs in the terminal ileum and may include the ascending colon with associated an associated inflammatory phlegmon or fistula. Right hemicolectomy for Crohn’s is performed when the disease is refractory to medical therapy. Right-sided diverticulitis: occurs uncommonly in the U.S. population and it is felt to arise as a congenital lesion occurring more commonly in Asian patients. It is commonly misdiagnosed as acute appendicitis. Ischemic colitis: uncommonly affects the right colon in isolation owing to its collateral blood supply; however may present with abdominal pain, bloating due to stricture, or hematochezia.
Cecal volvulus: caused by a twist (typically clock-wise) of the terminal ileum and colonic mesentery around fixed retroperitoneal attachments, presents with acute abdominal pain and obstructive symptoms.
Neoplastic pathology
Endoscopically unresectable polyps should be treated with colectomy. As they have potential to harbor malignant foci not detected on biopsy, they should be managed according to oncologic principles. Right-sided polyps include high-risk adenomas with high-grade dysplasia or villous components, large hyperplastic polyps, or sessile serrated adenoma/polyps (SSA/Ps).
Malignancy is the most common indication for laparoscopic right hemicolectomy. Equivalent outcomes to open resection have been demonstrated in large multi-center randomized controlled trials.2, 3, 4, 5, 6 A bulky cancer or one that has invaded into adjacent organs should be resected en bloc with associated tissues and may be considered for open resection.
Adenocarcinoma: The location with respect to the anatomy of the blood supply determines the extent of bowel resection.
Carcinoid: Right colectomy is indicated for carcinoid tumors of the terminal ileum or appendix when 2 cm or greater. Colectomy is also indicated for adverse features such as goblet cell carcinoid histology or presence of lymphovascular or perineural invasion.
PATIENT HISTORY AND PHYSICAL FINDINGS
Adenocarcinoma patients are commonly asymptomatic but can present with anemia, melena, altered stool patterns (diarrhea), pain, and weight loss.
A thorough history and physical examination is essential for identifying candidates for laparoscopic surgery. Several patient factors that can affect the feasibility of laparoscopic resection are shown in Table 1. Patient characteristics or underlying disease issue may preclude safety of the laparoscopic approach or greatly increase the operative difficulty and time and these factors should be considered when making the decision to proceed with laparoscopy and during operative planning.
Obesity poses unique challenges during laparoscopic hemicolectomy. The ease of finding the correct plane and the central vascular anatomy is greatly diminished in obese patients. Patient positioning may also be impacted by obesity as obese patients may not tolerate extreme Trendelenburg, reverse Trendelenburg, or side to side positioning. In addition, obesity has been associated with a higher risk for conversion to open surgery. Despite these challenges, patients who are obese have increased risk for morbidity such as wound infection when compared to nonobese patients and thus may derive significant benefit from laparoscopic surgery.
Patients with decreased cardiac output may not tolerate increased intraabdominal pressures resulting in decreased venous return secondary to pneumoperitoneum.
Intraabdominal adhesions caused by prior surgery may preclude laparoscopy. Laparoscopic lysis of adhesions may be
performed, although surgeon experience and the extent of adhesions should be considered.
Patients with nutritional deficiencies and impaired healing, such as those on high-dose steroids, recent immunomodulators, or systemic chemotherapy, are at higher risk for anastomotic failure. In those patients with ongoing life-threatening illnesses, ileocolonic anastomosis should be deferred in favor of end ileostomy. An ileocolostomy should not be performed in patients with hemodynamic instability.
Table 1: Patient Factors that Can Affect the Feasibility of Laparoscopic Resection | |||||||
|---|---|---|---|---|---|---|---|
|
DIAGNOSTIC STUDIES
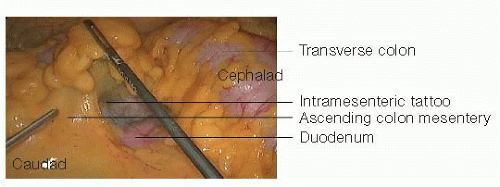
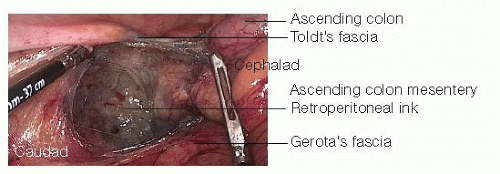
Colonoscopy: All tumors should be localized, biopsied, and tattooed prior to embarking on laparoscopic surgery. Tattooing allows for intraoperative localization of the tumor, although it may be faint when localized to the mesenteric border (FIG 1). The tattoo can also be on the retroperitoneal surface and not seen (FIG 2). Synchronous tumors (present in 3% to 5% of patients with colon cancer) and unresected polyps should be noted and considered in the treatment plan.7 Colonoscopy may not be possible in patients with a complete obstruction. In these patients, intraoperative palpation of the entire colon should be performed to assess for secondary lesions. After recovery from surgery, a short interval completion colonoscopy should be performed.
CT colonography/enterography: Can be useful in patients not amenable to colonoscopy. Use of CT enterography provides additional information of the small intestines in patients with Crohn’s disease that may alter surgical strategy.
CT scan of the abdomen and pelvis: In inflammatory bowel disease patients, CT scan provides information pertaining to the extent is of colitis, presence of a fistula, and/or abscess. In patients with malignancy, CT scans of the chest, abdomen, and pelvis should be performed to assess for pulmonary, hepatic, and lymphatic metastasis as well as infiltration of the primary tumor into adjacent structures.8
SURGICAL MANAGEMENT
Preoperative Planning
Appropriate preoperative antibiotic coverage before incision has been shown to decrease the risk of surgical site infections, but courses of antibiotics greater than 24 hours are actually associated with worse outcomes.9
Patient Positioning
The patient is positioned supine and secured with Trendelenburg straps on the ankles (FIG 3). If an extended right hemicolectomy will be performed, the patient may be placed in a lithotomy position to facilitate the mobilization of the splenic flexure, if necessary.
Gravity is the single greatest facilitator of exposure during colectomy. During the course of the case, the patient may be placed in steep Trendelenburg, reverse Trendelenburg and rotated right side up. For this reason, the patient must be secured to be operating table and a variety of devices have been used to secure the patient. We prefer to use ankle and chest straps, but commercially available foam pads placed under the patient to prevent slippage may also be used. We avoid using pads of beanbags placed above the shoulder that can cause brachial plexus injuries.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree