Laparoscopic Partial Colectomy
John C. Byrn
All benign and malignant indications for colectomy can be approached laparoscopically. Because it is difficult to palpate lesions, it is best to precisely localize the pathology before surgery (especially for smaller lesions). In contrast to open colon resection, laparoscopic colectomy is commonly performed from the “medial to lateral” approach described here. This is easier than the older “lateral to medial” approach because the mobilized colon does not obscure laparoscopic view.
SCORE™, the Surgical Council on Resident Education, classified laparoscopic partial colectomy as an “ESSENTIAL COMMON” procedure.
STEPS IN PROCEDURE
Right Colon Resection
Supine position, patient secured to bed
Trocar sites: Umbilical, suprapubic, left lateral to the umbilicus
Perform thorough laparoscopic exploration
Trendelenburg position with right side up table tilt
Place cecum and right colon mesentery on stretch to identify ileocolic artery (ICA)
Create a plane between ICA and retroperitoneum identifying duodenum
Ligate the ICA with LigaSure
Incise line of Toldt with right colon retracted medially
Mobilize colon from lateral attachments re-entering plane of medial dissection and re-identify duodenum
Place patient in reverse Trendelenburg position
Take hepatic flexure attachments medial to lateral after entering lesser sac and identifying transverse colon mesentery
Extend umbilical port incision to create a 3- to 5-cm incision
Exteriorize the right colon
Resect and control right branch of middle colic extracorporeally
Perform extracorporeal anastomosis
Return anastomosis to abdomen
Close extraction and trocar sites
HALLMARK ANATOMIC COMPLICATIONS
Ureteral injury
Injury to duodenum (right colon)
Splenic injury (left colon)
Missed lesion (resection of wrong segment)
LIST OF STRUCTURES
Colon
Inferior epigastric artery and vein
Right Colon
Cecum
Ascending colon
Hepatic flexure
Duodenum
Line of Toldt
Ileocolic artery
Transverse Colon
Right middle colic artery and vein
Lesser sac
Omentum
Left Colon
Splenic flexure
Descending colon
Sigmoid colon
Line of Toldt
Splenic flexure
Sacral promontory
Ureters
Inferior mesenteric artery and vein
Right Colon Resection—Trocar Placement and Patient Positioning
Technical Points
Place the patient in the supine position. Carefully pad and tuck both arms, placing them in a neutral “thumbs up” or slightly supinated position. This takes pressure off the ulnar nerve at the retrocondylar groove of the elbow.
Frequent, and sometimes extreme, patient positioning changes make cooperation with the anesthesia and nursing teams of utmost importance. All operating room participants should agree on positioning and padding, as the opportunity to reposition, after the patient is prepped and draped, may be limited.
Greater security in patient positioning can be obtained by using a “beanbag” (Olympus Vac Pac, Center Valley, PA). Secure this to the bed with cloth tape (to prevent rips in the beanbag). Place the beanbag flush with the perineum at the caudal extent of the operating room bed. Desufflate the bag with cranial edges “rolled” superiorly over the patient’s shoulders. This allows for very secure patient positioning, even with the obese patient in the steep Trendelenburg position.
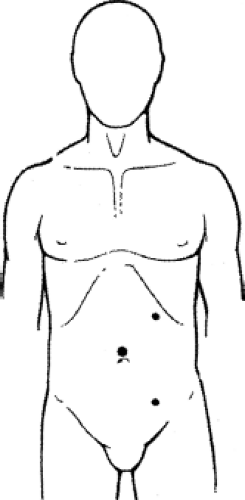
A three-trocar technique is used (Fig. 100.1). Place a 12-mm trocar at the superior aspect of the umbilicus, to accommodate a 10-mm, 30-degree laparoscope, using a Hasson technique. Place two 5-mm trocars: One in the midline suprapubic region, and the other in the left lower quadrant, but more precisely lateral to the umbilicus. True lower quadrant trocar positioning is comfortable when working on the ascending colon but will be self-limiting in terms of reach when mobilizing the hepatic flexure.
The surgeon and assistant both stand on the patient left, opposite the side of resection. Laparoscopic monitors are placed at surgeon “eye level” at about the level of the patient’s umbilicus.
Right Colon Resection—Mobilizing the Colon
Technical Points
Place the patient in Trendelenburg position with slight right side up tilt. Grasp the cecum and retract it toward the anterior abdominal wall. Note that the ICA is thus placed on stretch within its mesentery, facilitating identification (Fig. 100.2A,B). Create a mesenteric window below the artery. This will allow identification of the duodenum in the retroperitoneum and ensure a safe plane prior to a “high” ligation of the ICA. It is not necessary to look for the ureter at this stage of the
dissection. Take the major vascular pedicles of the colon preferentially with the 5-mm LigaSure (Covidien, Mansfield, MA). Carry this medial dissection cephalad toward the liver underneath the hepatic flexure and laterally to the white line of Toldt.
dissection. Take the major vascular pedicles of the colon preferentially with the 5-mm LigaSure (Covidien, Mansfield, MA). Carry this medial dissection cephalad toward the liver underneath the hepatic flexure and laterally to the white line of Toldt.
Next, incise the line of Toldt along the cecum or ascending colon sharply or with an energy device. The hepatic flexure can be mobilized considerably from the lateral perspective but when the dissection becomes difficult, it is best to turn one’s attention to the gastrocolic omentum and enter the lesser sac. This shift to working above the transverse colon is aided by placing the position in to reverse Trendelenburg position. Enter the lesser sac and then complete the mobilization of the hepatic flexure completely from medial to lateral. The right colon should now be fully mobilized and the duodenum should be in view.
Place the transverse mesocolon on stretch and lift it up off the retroperitoneum and the root of the small bowel mesentery. The right branch of the middle colic artery is then safely taken with the duodenum in view. This vessel can also be ligated extracorporeally during specimen extraction and resection.
Anatomic Points
With the lateral attachments of the colon incised along the line of Toldt gentle medial retraction on the right colon will often lead to efficient, full mobilization. The duodenum should be viewed from lateral to medial when the plane of medial dissection is reentered during this mobilization.
When mobilizing the hepatic flexure the division of the omentum or gastrocolic omentum toward the midline allows easy entry into the lesser sac preventing inadvertent injury or uncontrolled division of the transverse mesocolon.
The duodenum should again be in view from a superior–lateral to medial vantage after the hepatic flexure is fully mobilized. This does not require ligating the right branch of the middle colic artery and vein. Identification of the duodenum medially during isolation and ligation of the ICA, lateral to medial when mobilizing the lateral right colon attachments, and then again superior–lateral to medial after hepatic flexure takedown are key views for safe right colon mobilization.
Right Colon Resection—Extracorporeal Resection and Anastomosis
Technical Points
Now extend the umbilical trocar site under direct vision to create the extraction site. Place a wound protector and use a Babcock clamp to easily grab the mobilized cecum under direct vision. Exteriorize the bowel.
Identify healthy, well-perfused transection sites on the ileum and colon where an anastomosis can be created without undue tension. For a stapled anastomosis, use a linear cutting stapling device to transect the ileum and the colon and allow removal of the surgical specimen (Fig. 100.3A) If the right branch of the middle colic artery and vein were not ligated intracorporeally, then clamp and tie these before resecting the specimen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree