Laparoscopic Paraesophageal Hernia Repair
Hui Sen Chong
Samy Mokhtar Maklad
Paraesophageal hiatus hernias allow the stomach or other viscera to ascend through the hiatus into the mediastinum (see Chapter 52, Fig. 52.1). Laparoscopic repair is increasingly the preferred method, as it has less morbidity when compared to the open abdominal and thoracic approaches. The minimally invasive technique for repair described in this chapter follows the same principles as the open repair described in Chapter 52. The key principle of a successful paraesophageal hernia repair is as follows: Complete reduction of herniated viscera, adequate mobilization of the esophagus to allow 3 cm of distal esophagus to lie without tension in the abdominal cavity, tension-free crural repair, and an antireflux procedure. In this chapter we will only discuss the technical aspect of the laparoscopic paraesophageal repair; please consult Chapter 52 for the relevant anatomic points.
SCORE™, the Surgical Council on Resident Education, classified laparoscopic repair of paraesophageal hernia as an “ESSENTIAL UNCOMMON” procedure.
Steps in Procedure
Obtain five-port laparoscopic access
Retract left lobe of liver exposing hiatus
Incise gastrohepatic and phrenoesophageal ligaments
Excise hernia sac and mediastinal adhesions
Reduce herniated viscera from chest
Expose and define right and left crura
Divide the short gastric vessels
Mobilize distal esophagus and create retroesophageal window
Assess esophageal length and need for modified Collis gastroplasty
Approximate esophageal hiatus with interrupted permanent sutures
Consider the need for biological mesh reinforcement
Perform Nissen fundoplication with bougie in place
Perform intraoperative esophagogastroduo/deno/scopy (EGD) if needed
HALLMARK ANATOMIC COMPLICATIONS
Injury to:
Accessory or replaced left hepatic artery
Left gastric artery
Stomach
Esophagus
Vagus nerve
Spleen
Heart, lung, or aorta
Inadequate mobilization of esophagus
Inadequate closure of hiatus
Excessively tight wrap
Herniation through hiatal defect
LIST OF STRUCTURES
Diaphragm
Left and right crura
Esophageal hiatus
Gastrohepatic ligament
Accessory or replaced left hepatic artery
Gastrosplenic ligament
Short gastric arteries and veins
Fundus of the stomach
Pleura
Aorta
Esophagus
Left and right vagus nerves
Left lobe of liver (segments II and III)
Caudate lobe of liver (segment I)
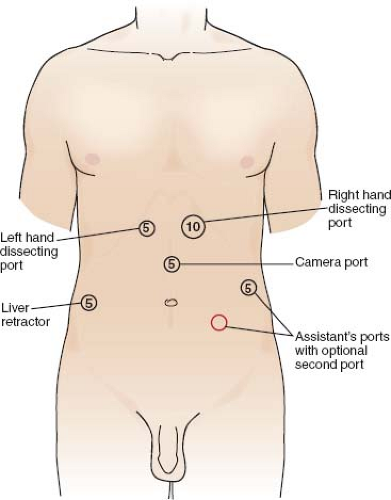
Patient Positioning and Laparoscopic Port Placement (Figs. 54.1 and 54.2)
Technical Points
Position the patient in the modified lithotomy or split leg position with both arms extended. Perioperative antibiotics and SQ heparin should be administered. After padding all pressure points and securing the patient, a total of five laparoscopic ports using a combination of 5-mm and 10-mm trocars are positioned as follows. One supraumbilical 5-mm port to accommodate a 5-mm 30-degree laparoscope. Place this port about halfway between the xiphoid and the umbilicus, just slightly off to the left of the midline to avoid the falciform ligament. Place a 5-mm port at the right anterior axillary line, about 3 to 4 inches below the costal margin to accommodate a self-forming liver retractor.
Inspect the abdomen in the usual fashion. Place a liver retractor to elevate the left lobe of the liver to expose the hiatus and secure it to a stationary holding device (Fig. 54.2). In most patients, the liver retractor should provide adequate hiatal exposure and the left triangular ligament can be left in place. Next, position a 5-mm right and a 10-mm left subcostal port along the midclavicular lines. These are used as the main dissecting ports and should be placed as cephalad as possible to allow for dissection in the mediastinum. Place the 5-mm right subcostal port just to the left of the falciform ligament and below the lower edge of the elevated left liver lobe. Lastly, place a 5-mm port in the left anterior axillary line for the assistant.
If an additional port is needed for retraction, a second 5-mm port may be placed in the left lower quadrant region, just slightly lower than the camera port. The surgeon stands in between the legs to allow for ergonomic dissection, while the assistant stands on the left side of the table as shown in Chapter 46, Figure 46.1C.
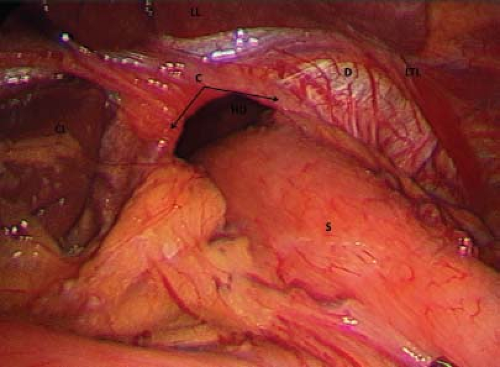
Hiatal Dissection and Reduction of Gastric Fundus (Fig. 54.3)
Technical Points
Using atraumatic graspers passed through the main dissecting ports, gently reduce the easily reducible portion of the herniated stomach back into the abdominal cavity. The assistant provides lateral retraction to the herniated stomach while the surgeon divides the gastrohepatic ligament using the Harmonic scalpel (Fig. 54.3). The gastrohepatic ligament is the avascular tissue that joins the lesser curvature of the stomach to the liver. In 10% to 15% of the population, a replaced or accessory left hepatic artery arising from the left gastric artery may be present within the gastrohepatic ligament. It is easily identified as the vessel that travels horizontally within the gastrohepatic ligament. Oftentimes, the gastrohepatic ligament can be divided with the Harmonic scalpel, cephalad to the aberrant left hepatic artery. This maneuver will allow the artery to fall away from the surgical field while maintaining exposure of the hiatus. Take care also to avoid injury to the left gastric artery, which lies just posterior to the gastrohepatic ligament.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree