Laparoscopic Pancreaticojejunostomy
Steven J. Hughes
DEFINITION
Laparoscopy indicates the use of a camera combined with minimal access techniques to perform surgical, abdominal procedures.
Pancreaticojejunostomy (PJ) is the operative anastomosis of a remnant pancreas (distal pancreas) to a limb of jejunum to restore continuity of pancreatic secretions into the intestinal tract. This procedure is necessary following pancreaticoduodenectomy.
PATIENT HISTORY AND PHYSICAL FINDINGS
Pancreatic texture will vary depending on the underlying indication for pancreaticoduodenectomy as well as associated patient factors.1 The pancreatic duct may also vary in size, depending on whether the duct has been previously obstructed, has been involved in intraductal papillary mucinous neoplastic changes, or is of normal caliber.
The major risk of PJ is leakage of pancreatic secretions leading to abscess or fistula. A classification scheme for the severity of this complication has been characterized.
This complication is less frequent when the pancreas is firm in texture, thus providing a substrate that firmly anchors sutures and is not prone to laceration.
SURGICAL MANAGEMENT
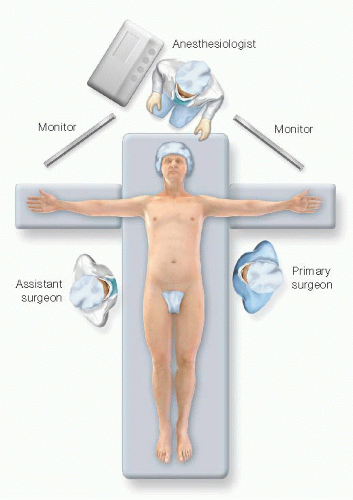
Positioning
The patient is positioned supine; tucking of the arms is not necessary (FIG 1). Some surgeons prefer a “split-table” approach, where the surgeon is positioned between the patient’s legs.
Reverse Trendelenburg position facilitates the exposure. Thus, a footboard should be used.
TECHNIQUES
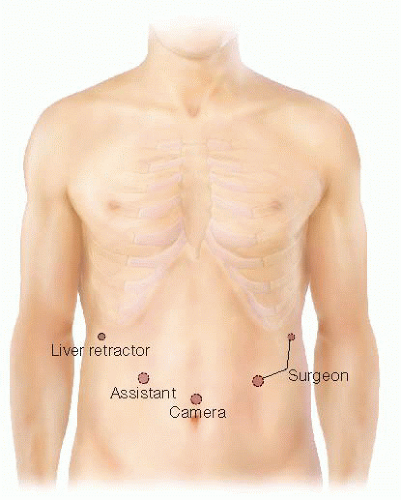
TROCAR PLACEMENT
Trocar placement is depicted in FIG 2. Five access points are the minimum required to perform the technique laparoscopically. A fixed retractor is placed in the far right port to elevate the left lobe of the liver and improve exposure to the pancreatic remnant. The other trocars are used for the camera, a first assistant, and the operative surgeon.
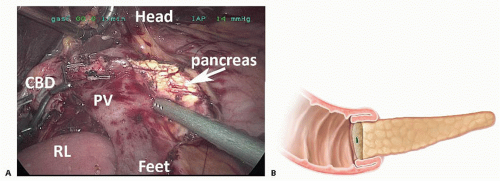
MOBILIZATION OF THE REMNANT PANCREAS
To complete the posterior suture row of the anastomosis, a minimum of 1 cm and ideally 2 cm of the remnant pancreas must be mobilized (FIG 3). Increased mobilization of the remnant pancreas facilitates elevation of the gland during the anastomosis and results in improved visualization.
The reconstructive limb should be fashioned focusing on adequate mesenteric length and preservation of the arterial and venous blood supply. A number of options regarding reconstructive anatomy are available. The author favors positioning the reconstructive limb posterior to the mesenteric vessels as a “neoduodenum.”2 Given the natural orientation of the mesentery of the proximal jejunum, this reconstructive approach minimizes the length of the mesentery necessary to perform the PJ in a tension-free environment. This approach also reduces the potential for internal hernia or other technical errors associated with creating a window in the transverse mesocolon. Importantly, this approach avoids excessive rotation of the jejunal limb behind the mesenteric vasculature.
TECHNIQUE 1: END-TO-END INTUSSUSCEPTING ANASTOMOSIS
The anastomosis is constructed with a running 4-0 polydioxanone suture on a vascular RB-1 needle. A double-armed suture measuring 40 cm in length (20 cm for each arm) is fashioned by tying two sutures together. The suture is placed through a 12-mm trocar and one arm is positioned out of the surgical field in the left upper quadrant. This arm will be used later for the anterior suture line. The staple line on the reconstructive limb of jejunum is removed using electrocautery.
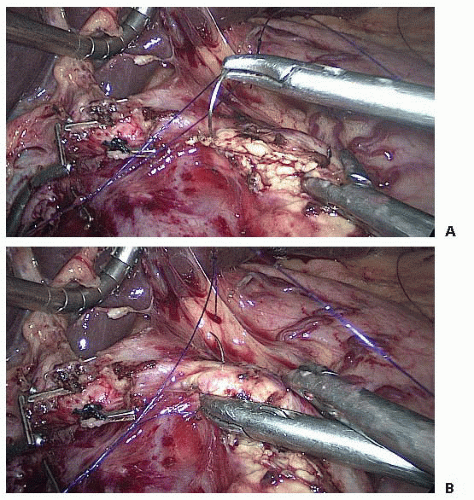
The anastomosis is initiated by placing the first suture in the reconstructive limb as shown in FIG 4. This will facilitate forehand suturing for the entire anastomosis and place the tension of posterior suture line on the serosa of the bowel rather than the soft parenchyma of the pancreas. This suture should be placed at the antimesenteric border of the reconstructive limb.
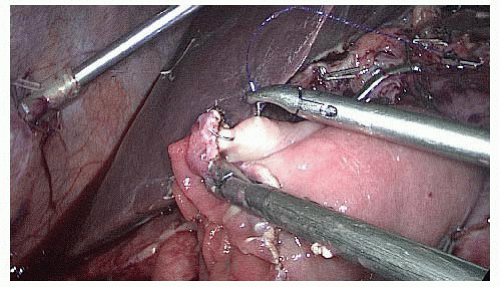
The first bite of the pancreatic parenchyma is placed back hand at the cephalad aspect of the remnant pancreas as depicted in FIG 5. This suture is typically oriented transverse to the longitudinal plane of the pancreatic remnant. Subsequent sutures in the pancreas will be oriented longitudinally.
The suture is then passed posterior to the suture that now bridges the bowel and the pancreas as shown in FIG 6. This maneuver is essential to prevent locking of the suture as the posterior suture line of the anastomosis is initiated.
An additional purchase of the reconstructive limb is taken and then the suture is “parachuted” down to appose the reconstructive limb to the remnant pancreas (FIG 7). Care should be taken to ensure that the knot securing the two arms of the suture is in good apposition to the serosa of the bowel. Failure to do so will subsequently impact the ability to obtain adequate tissue apposition at the cephalad aspect of the anastomosis with the first tissue bites of the anterior suture line.
The first assistant provides exposure and maintains tension on the suture line by grasping the suture with an
atraumatic grasper approximately 1.5 to 2 cm above suture line as shown in FIG 8. The posterior suture line is then run continuously (FIG 9). The operating surgeon sets the tension of the suture on the tissue after each bite of jejunum, and then passes the suture on tension to the first assistant. At the caudad aspect of the pancreas, the suture is held by the placement of a Lapra-Ty™ (FIG 10).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree