Laparoscopic Low Anterior and Abdominoperineal Resection
Adam J. Dinnewitzer
Steven D. Wexner
Indications for laparoscopic colorectal surgery do not differ from those for open procedures. The only difference should be the method of access. As in open procedures, laparoscopic abdominoperineal resection is appropriate only for carcinomas that invade the anal sphincter or that are so close to the sphincter that a clamp or a stapler cannot be placed 2 cm or more to the distal edge of the tumor. Laparoscopic low anterior resection is appropriate for cancers in the mid (5 to 10 cm from the dentate line) or low rectum (less than 5 cm from the dentate line); in these cases, a total mesorectal excision with a coloanal anastomosis should be performed.
Preoperative evaluation, mechanical and antibiotic bowel preparation, and thromboembolic prophylaxis are also identical to those measures employed for open procedures. Preoperatively, an enterostomal therapist selects and marks the preferred site for a temporary or permanent stoma.
Unlike laparoscopy for benign disease, the benefits of laparoscopy for cancer have not yet been proved. Therefore laparoscopic surgery for curative resection of rectal cancers should be done only in the context of a peer-reviewed externally monitored prospective randomized trial.
In this chapter, we describe both laparoscopic low anterior resection and laparoscopic abdominoperineal resection; use of a coloanal anastomosis as the intraabdominal component of the procedure is identical in both. Regardless of the procedure and technique, performance of a total mesorectal excision is of paramount importance in the cure of tumors in the lower two thirds of the rectum.
Steps in Procedure
Modified lithotomy position
Umbilical trocar site; thorough exploration of abdomen
Additional trocar sites: right lower quadrant, right paraumbilical, left paraumbilical, or right upper quadrant
Steep Trendelenburg position with table tilted to the right
Grasp sigmoid colon and retract medially
Incise line of Toldt and mobilize colon medially
Identify and protect ureter
Mobilize splenic flexure without pulling on spleen
Divide inferior mesenteric vessels
Elevate uterus and adnexa in female
Grasp rectum and retract cephalad and anteriorly
Incise peritoneum laterally and anteriorly
Dissect in avascular plane along iliac vessels (preserving ureters) and presacral space
Anteriorly the plane should be just deep to vaginal wall (female) or seminal vesicles (male)
For Low Anterior Resection, Divide Rectum at Chosen Point with Linear Stapler
Lengthen left or right lower quadrant point to 5 cm, place plastic sleeve, and remove specimen
Create J-pouch with linear stapler
Return colon to abdomen and close incision, reestablish pneumoperitoneum
Create stapled anastomosis with circular stapler, inserted transanally
Consider loop ileostomy
Close trocar sites in usual fashion
For Abdominoperitoneal Resection
Complete mobilization of rectum to levator sling
Perineal phase of operation is performed as usual
Remove specimen through perineal wound
Create end colostomy
Place drain
Close trocar sites in usual fashion
Hallmark Anatomic Complications
Injury to ureters
Injury to spleen
Bleeding from presacral venous plexus (improper dissection plane)
Laparoscopic Low Anterior Resection
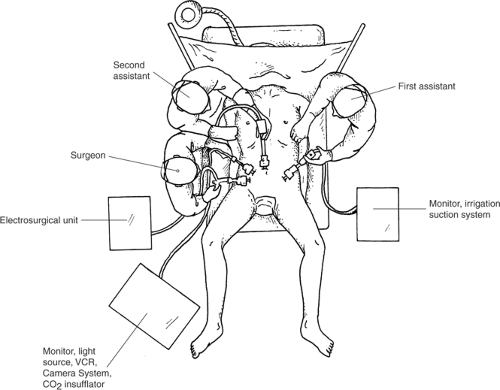
Preoperative Setup and Trocar Placement (Fig. 84.1)
Technical Points
Place the patient in a modified lithotomy position with the hips and knees gently flexed at a maximum 15-degree angle. Greater elevation of the thighs may not allow the surgeon to move the instruments freely. The buttocks should extend slightly over the end of the operating table. This position gives proper access to the anus for endoscopy and insertion of a circular stapling device and also allows access to the perineal region in case of abdominoperineal resection. Place the right arm of the patient alongside the trunk (rather than out on an armboard) to allow room for the surgeon and second assistant, who stand on the right side of the patient. Place an orogastric tube and a urinary catheter to minimize the risk for gastric or bladder injury, respectively, during trocar insertion. Prepare and drape the abdomen and perineal region for an open procedure for the eventuality that the laparoscopic procedure cannot be safely completed. The surgeon stands on the right side of the patient, the first assistant surgeon on the left, and the second assistant, who controls the camera, to the left of the surgeon.
A CO2 pneumoperitoneum of 12 to 15 mm Hg is established in the usual fashion, through a small vertical infraumbilical incision. A 0- or 30-degree laparoscope is then introduced, and the abdomen is thoroughly explored to assess other pathology and to determine any metastatic dissemination. To inspect the liver, the patient is brought into a steep reverse Trendelenburg position; if the technology is available, a laparoscopic ultrasound of the liver should be performed.
If the proposed operation is deemed feasible, the other ports will be positioned. The operation is facilitated by the camera and the instruments being interchangeable to all ports. For this reason, only 10- to 12-mm trocars are used; three operating port sites are usually sufficient. Place the additional trocars under direct endoscopic visualization in the right lower quadrant and at the level of the umbilicus, both along the right midclavicular line. Another port is inserted in either the left midclavicular line, also at the level of the umbilicus, or in the right upper quadrant in the midclavicular line. The port positioning takes into account the patient’s anatomy, the location of the incision for specimen retrieval, and the site of any planned stoma.
The following additional instruments are required:
Four 10- to 12-mm trocars with reducer caps
Ultrasonic scalpel
One 10-mm bowel clamp
Two 10-mm Babcock graspers
Both 30- and 45-mm endoscopic linear cutting staplers
A 29-mm or 33-mm endoscopic curved intraluminal stapler
A 75-mm linear cutting stapler
A 5-inch plastic wound protector
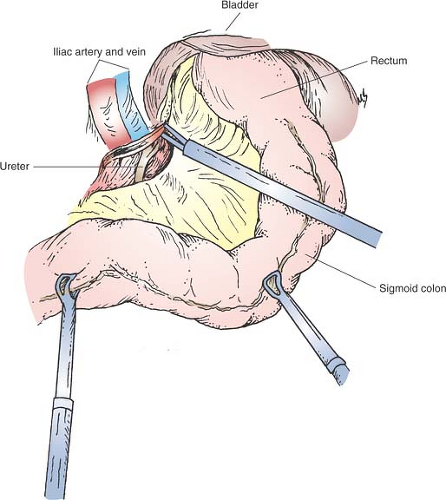
Mobilizing the Sigmoid and Descending Colon (Fig. 84.2)
Technical Points
Place the patient in a steep Trendelenburg position with the table tilted to the right side so that the small bowel gravitates toward the right upper quadrant of the abdomen and no retraction to the small bowel is required. Gently grasp the sigmoid colon with a Babcock clamp through the right paraumbilical port and move the bowel to the patient’s right side. This maneuver places traction on the posterior peritoneum overlying the iliac vessels. Incise the peritoneum with the ultrasonic scalpel placed through the right lower quadrant port. Sequentially slide the ultrasonic scalpel under the peritoneum, and advance it down the pelvic sidewall toward the anterior peritoneal reflection, using it to push the mesorectum and mesosigmoid medially away from retroperitoneal structures. Identify the ureter as it crosses the iliac vessels and trace it proximally as far as possible. Continue this separation of the sigmoid colon from the lateral wall cephalad along the descending colon until the splenic flexure is reached.
Anatomic Points
The abdominal and pelvic part of the ureter lies in extraperitoneal areolar tissue. The abdominal part, which descends on the medial part of the psoas major muscle, enters the lesser pelvis anterior to either the end of the common or the beginning of the external iliac vessels. The left ureter lies beneath the root of the sigmoid mesocolon. The right ureter lies behind the lower part of the mesentery and the terminal ileum. In the pelvis, the ureter is anterior to the internal iliac artery and covered by the parietal endopelvic fascia. Laterally, it lies on the fascia of the musculus obturator internus. In males, the ureters pass between the internal iliac vessels and the ascending vas deferens. Then they turn anteriorly, pass along the levator ani, and penetrate the base of the bladder in front of the seminal vesicles. In females, the pelvic part at first has the same relations as in males, but anterior to the ureters lay the ovaries. At the pelvic floor, the ureter turns anteriorly on the levator ani, turns forward slightly above the lateral vaginal fornix, and then inclines medially to reach the bladder.
Mobilizing the Splenic Flexure (Fig. 84.3)
Technical Points
Place the patient in a steep reverse Trendelenburg position. This allows the transverse colon and viscera to fall away from the spleen and stomach. While the assistant retracts the splenic flexure toward the umbilicus with the Babcock clamp, separate the mesentery of the descending colon from Gerota’s fascia until the splenic flexure is reached.
Next, approach the splenic flexure along the transverse colon. Displace the greater omentum toward the stomach and retract the transverse colon caudad to expose the avascular plane between the omentum and the transverse colon. Incise this avascular plane with the ultrasonic scalpel to enter the lesser sac and continue the dissection until the splenocolic ligament is completely divided. The sigmoid colon, the descending colon, and the transverse colon have now been fully mobilized to the midline.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree