Laparoscopic Inguinal Hernia Repair
Laparoscopic inguinal hernia repair takes a totally different approach from open repair. It is most nearly analogous to a preperitoneal open repair, sometimes termed the Nyhus repair, performed with mesh. The logic is similar to that employed during laparoscopic ventral herniorrhaphy: because the problem is a weakness in the transversalis fascia (or a persistently patent processus vaginalis), approach the defect from inside. Peritoneum is stripped from the region, and the defect is repaired with a large sheet of prosthetic mesh. Intraabdominal pressure holds the mesh buttressed against the muscular and aponeurotic layers of the abdominal wall, which are not dissected. Tacks are placed to secure the mesh in place. The anatomy that is stressed for this repair is very different than that stressed in Chapter 94. There is little emphasis on the muscular and aponeurotic layers of the abdominal wall. Rather, avoiding complications during these procedures requires intimate knowledge of the anatomy of crucial nerves and blood vessels that must be avoided when the mesh is secured. Major complications of the procedure include vascular injury and neurapraxia. The procedure may be done transabdominal preperitoneal (TAPP) or totally extraperitoneal (TEP). In this chapter, the transabdominal approach is shown first, followed by the modification employed for TEP.
Steps in Procedure
Transabdominal Preperitoneal (TAPP) Approach
Supine position
Trocars at umbilicus and left and right paraumbilical
Abdominal exploration
Confirm presence of hernia defect or defects
Incise peritoneum from median umbilical ligament to anterosuperior iliac spine, approximately 2 cm cephalad to hernia
Develop flaps and reduce sac
Tailor large piece of mesh and pass into abdomen
Secure mesh with staples or tacks along superior edge of mesh
Close peritoneum over mesh
Close trocar sites in usual fashion
Total Extraperitoneal Repair (TEP)
Initial entry into preperitoneal space via open technique
Bluntly dissect preperitoneal fat from fascia
Use dissecting balloon to develop the space
Place additional trocars
Separate sac from underlying structures; ligate large indirect sac if necessary
Place mesh as noted above
Close trocar sites in usual fashion
Hallmark Anatomic Complications
Injury to lateral femoral cutaneous nerve
Injury to anterior femoral cutaneous nerve
Injury to femoral nerve
Injury to genitofemoral nerve (femoral or genital branches)
Injury to external iliac artery or vein
Injury to aberrant obturator arteries
Injury to bladder (if prior surgery in the preperitoneal space)
List of Structures
Peritoneum
Transversalis fascia
Patent processus vaginalis
Ductus deferens
Seminal vesicles
Round ligament of uterus
Bladder
Deep (internal) inguinal ring
Medial Umbilical Ligament (Fold)
Urachus
Median umbilical ligaments (folds)
Obliterated umbilical artery
Lateral Umbilical Ligaments (Folds)
Inferior epigastric artery and vein
Supravesical fossa
Medial umbilical fossa
Lateral umbilical fossa
Hesselbach’s triangle
Iliopubic tract
Femoral canal
Cooper’s ligament
Conjoint tendon
Arch of aponeurosis of transversus abdominis
Lateral femoral cutaneous nerve
Anterior femoral cutaneous nerve
Femoral nerve
Genitofemoral Nerve
Femoral branch
Genital branch
Ilioinguinal nerve
Iliohypogastric nerve
External iliac artery and vein
Femoral artery and vein
Internal iliac artery and vein
Obturator Artery
Aberrant obturator artery
Prevesical space (of Retzius)
The muscular and aponeurotic structures of the anterior abdominal wall appear different when viewed from inside with the peritoneum removed (see part A of the orientation figure). Note how the ductus (or vas) deferens enters through the deep inguinal ring and then passes inferiorly and medially to join the seminal vesicles in the region of the base of the bladder. The internal spermatic vessels pass from lateral to medial and ascend to pass through the deep inguinal ring. The inferior epigastric vessels ascend and pass medially, defining the lateral border of Hesselbach’s triangle. The medial umbilical ligaments, the obliterated remnants of the umbilical arteries, form useful visual landmarks. The median umbilical landmark is rarely seen. Part B of the orientation figure shows peritoneum intact on the right side, demonstrating the peritoneal folds and visual landmarks with peritoneum intact. On the left side, the peritoneum has been removed to reveal underlying structures of significance. Note the iliopubic tract, the femoral canal, Cooper’s ligament, and the arch of the aponeurosis of the transversus abdominis. Contrast this view with the anterior and posterior views shown in the orientation figure for Chapter 94.
Multiple nerves and vessels, most never encountered during open inguinal or femoral herniorrhaphy, are at risk during laparoscopic repair. Nerves include the lateral femoral cutaneous nerve, the anterior femoral cutaneous nerve, the femoral nerve, the femoral branch of the genitofemoral nerve, and the genital branch of the genitofemoral nerve. The vascular structures at risk include the external iliac artery and vein and aberrant obturator arteries. The latter, also termed the “artery of death,” is a potential pitfall when a femoral hernia is repaired from above (see Fig. 94.8 in Chapter 94).
Two triangles, which lie together to form a rough trapezoid, encompass the majority of these structures and form a useful mnemonic device (see part C of the orientation figure). The “triangle of pain” is bounded by the iliopubic tract superiorly, the testicular vessels medially, and the cut edge of the peritoneum inferiorly. It contains most of the nerves previously mentioned. The “triangle of doom,” bounded by the testicular vessels laterally, the ductus deferens medially, and the cut peritoneal edge inferiorly, contains the vessels. Extreme care must be exercised while dissecting in these triangles, and no staples or other fixation devices should be placed in these regions.
TAPP—Orientation and Initial View of Male and Female Pelvis (Fig. 95.1)
Technical Points
Position the patient supine. Place three ports as shown (Fig. 95.1A). Use an angled (30- or 45-degree) laparoscope for better visualization of the inguinal region. Note that in the male, the ductus deferens and inferior spermatic vessels form the apex of a triangle that points to the internal inguinal ring (Fig. 95.1B). Normally, the peritoneum over this region is smooth, or, at most, a tiny dimple or crescentic fold will be seen at the internal ring. In the female, the round ligament is seen to terminate in the internal ring (Fig. 95.1C). Confirm the presence of a hernia or of multiple defects by noting outpouchings in the peritoneum either medial (direct) or lateral (indirect) to the inferior epigastric vessels (Fig. 95.1D, E).
Anatomic Points
As the parietal peritoneum covers the undersurface of the anterior abdominal wall and pelvis, underlying structures tent it up, creating five peritoneal folds. These form visual landmarks useful to the laparoscopic surgeon.
In the midline, the remnant of the obliterated urachus links the umbilicus with the dome of the bladder. Although this median umbilical fold is shown in parts A and B of the orientation figure, it is rarely actually visible to the laparoscopic surgeon, perhaps because it is so close to the umbilically placed laparoscope. The space above the bladder is termed the supravesical fossa.
The paired medial umbilical ligaments are much more obvious. These contain the obliterated remnants of the umbilical arteries. They lead from the umbilicus to the internal iliac arteries bilaterally. The region of interest to the laparoscopic hernia surgeon lies just lateral to the medial umbilical ligaments.
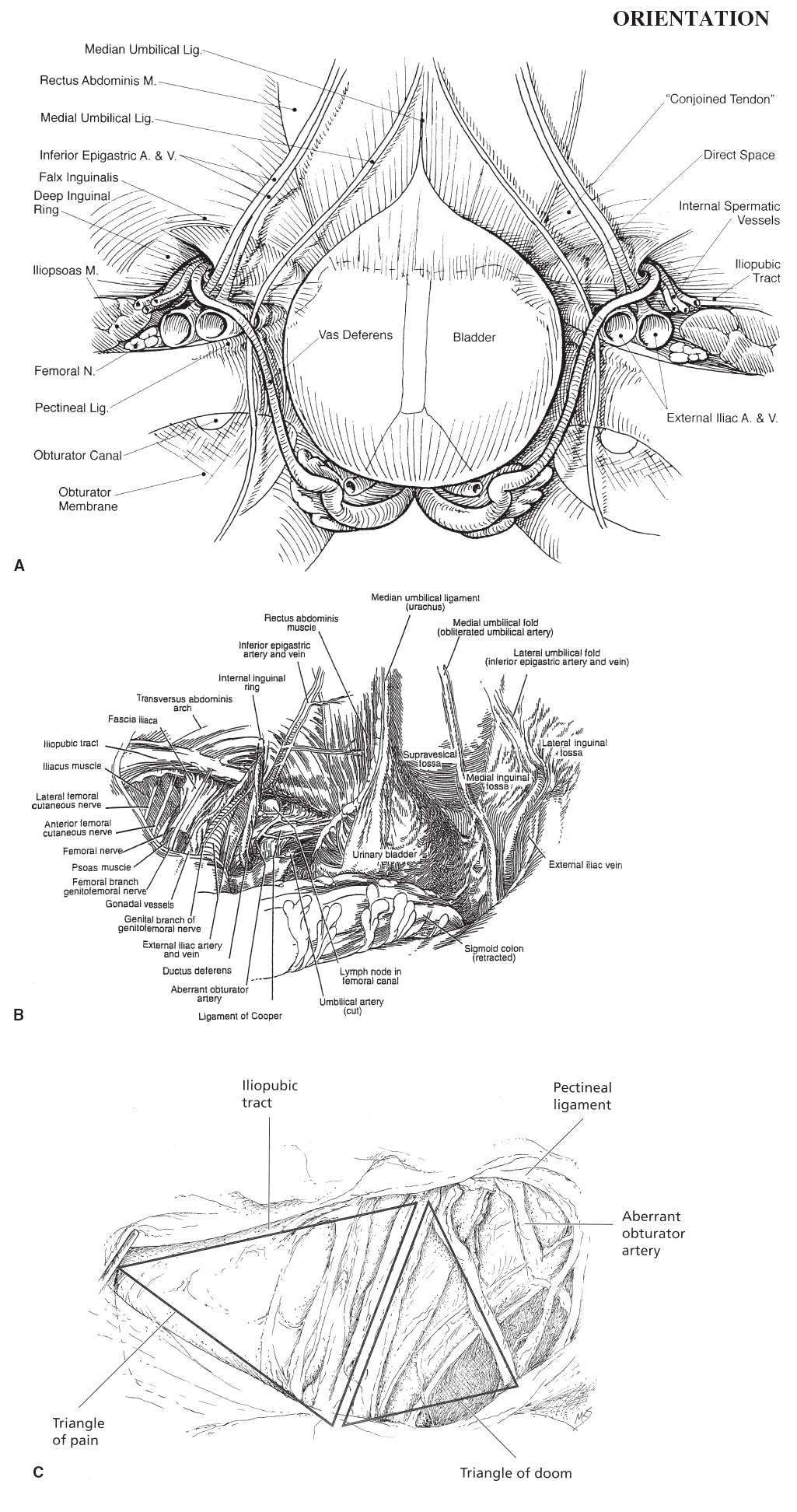 |
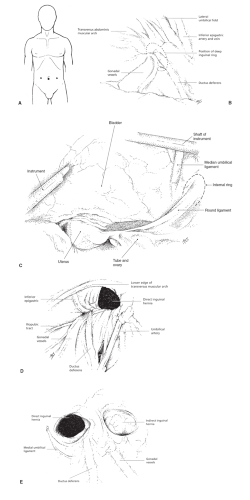 Figure 95-1 TAPP—Orientation and Initial View of Male and Female Pelvis (B,D,E from Colborn GL, Brick WG. Inguinal region. In: Scott-Conner CEH, Cuschieri A, Carter FJ, eds. Minimal Access Surgical Anatomy. Philadelphia: Lippincott Williams & Wilkins; 2000:239–266, with permission; C from Hedican SP. Pelvis. In: Scott-Conner CEH, Cuschieri A, Carter FJ, eds. Minimal Access Surgical Anatomy. Philadelphia: Lippincott Williams & Wilkins; 2000:211–238, with permission.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|