A colostomy is a surgically created communication through the body wall between the colon and the skin. There are several different kinds of colostomies, including the following:
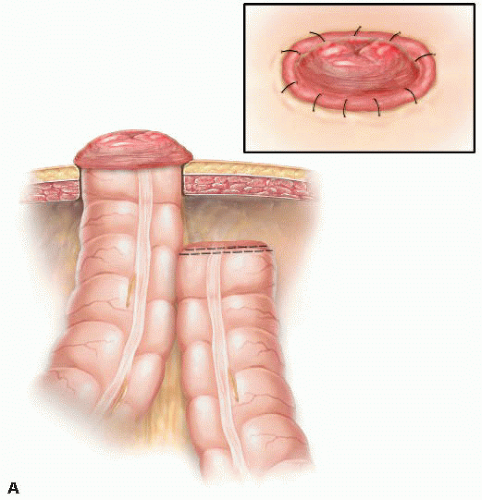
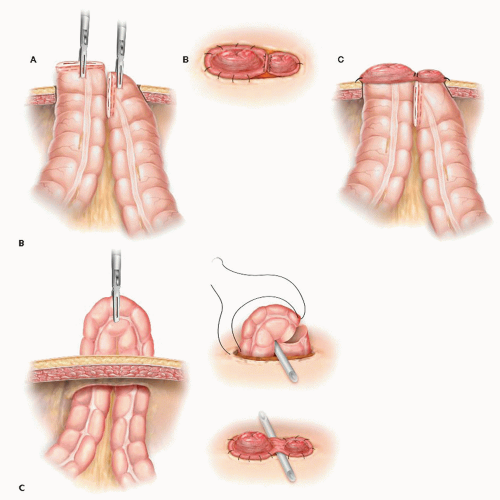
End colostomy: a colostomy in which a divided end of colon passes through the stomal trephine to open externally with a circumferential colocutaneous anastomosis (FIG 1A). A stomal trephine is a surgically created defect through layers of abdominal wall through which the colon passes to the external opening.
Double-barreled colostomy: a colostomy in which two divided ends of colon pass through the stomal trephine to open externally, each via a circumferential anastomosis (FIG 1B).
Loop colostomy: a colostomy in which a loop of colon passes through the stomal trephine to open externally via a colocutaneous anastomosis. A variable portion (usually 50% to 75% of the circumference) of the antimesenteric colonic wall is used for colocutaneous anastomosis. A variable portion (usually 25% to 50% of the circumference including the mesenteric border) of the colonic wall remains in continuity (FIG 1C).
Tube colostomy: a colostomy in which a prosthetic tube passes from the colonic lumen through the abdominal wall to open externally.
Diverting colostomies may be temporary or permanent. The possibility and likelihood of a stoma reversal must be taken into consideration prior to its formation.
Diverting colostomies may be indicated by any combination of distally located pathology (i.e., malignancy, obstruction, sepsis, fistula, inflammatory bowel disease [IBD]), functional disorders (i.e., pelvic floor or anal sphincter dysfunction), or recent or concurrent surgical procedure.
Patient factors such as age, gender, body habitus, current medical comorbidities, and previous medical and surgical conditions along with psychological, social, and cultural issues must be elicited and taken into consideration.
Prior to embarking on reversal of colostomies, detailed knowledge is needed of the stoma creation and other operative procedures. Details such as type of stoma, resection of colon, peritoneal contamination, mobilization of splenic flexure, and marking of distal colon or rectum, if present, with a nonabsorbable suture are helpful in the operative planning process. In addition, up-to-date knowledge of the original pathology or indication necessitating formation of the stoma in the first instance is essential.
Physical examination primarily focused on the patient’s body habitus, abdominal contour, and presence of abdominal scars is important in the consideration of the type and site of the stoma to be formed.
Preoperative investigation will be directed toward the underlying condition necessitating fecal diversion to exclude pathology proximal and/or distal to the intended colostomy site.
Unrecognized Crohn’s colitis, ileocolonic IBD strictures, synchronous tumors or other pathology may result in stomal complications or failure.
Colonoscopy, computed tomography (CT) scan and/or colonic transit studies may help plan the type and site of stoma formation.
It is critical to determine preoperatively which section of colon is to be used and if an end, double-barreled, or loop colostomy is to be formed.
In the setting of proximal diversion for distal pathology, we prefer to use the sigmoid colon. Should this not be possible, we often opt for a diverting loop ileostomy. Alternatively, a transverse colostomy is an adequate option.
The decision-making process regarding formation of an end, double-barreled, or loop colostomy is more complex and is illustrated in Table 1.
Preoperative assessment and education, as well as preoperative stoma marking by an experienced stomal practitioner in conjunction with the surgeon, is highly recommended.
Identifying the optimal stomal site should involve assessment of the patient standing, sitting, and supine. Factors involved in stomal site assessment are also listed in Table 1.
Deep vein thrombosis (DVT) prophylaxis is recommended in the form of antithromboembolic compression stockings,
sequential compression devices, and/or prophylactic heparin or low-molecular-weight heparin (LMWH).
Table 1: Decision Making Regarding Stoma Site and Type
Stoma position
Preferable: readily visible, accessible, and transrectus
Avoid: skin creases, belt lines, scars/incisions, hernia, and bony prominences; lateral ostomies may interfere with arm motion while walking.
Sigmoid colostomy
Ideal site: LLQ, transrectus at a point one-third the distance between the umbilicus and the ASIS
Transverse colostomy
Ideal site: RUQ, transrectus at a point one-third from the distance between the umbilicus and the junction of the costal margin and midclavicular line.
Stoma type
End colostomy: preferable for permanent stomas. Technically easier to construct and associated with a reduced complication rate. Advantageous in the difficult-toconstruct stoma (e.g., the obese abdomen).
Double-barreled colostomy: usually reserved for stomas constructed during an operation in which a segment of colon has been resected and an anastomosis was not undertaken, but subsequent reversal is likely.
Loop colostomy: preferable for temporary stomas and/or when there is distal obstruction
Obese patients
Consider an end colostomy. Division of the colon and part of the mesentery will give more length and allow easier passage of the stoma through the ST.
Consider siting the stoma in the upper abdomen where there is thinner abdominal wall. (The lower abdomen adiposity is most pendulous.)
Visualization and therefore appliance manipulation is compromised if the stoma is situated on the underside of an adipose roll or pendulous abdomen.
ASIS, anterosuperior iliac spine.
A single 2-g dose of Cefoxitin is administered prior to incision unless contraindicated.
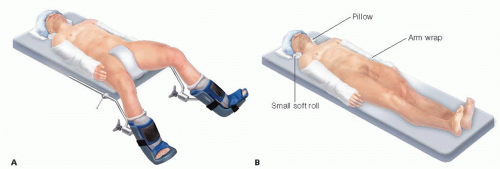
For creation of sigmoid colostomy and reversal of end colostomy, the patient is positioned in a modified Lloyd-Davies position (FIG 2A) on a nonslip pressure area care mat (Jelly Mat). The right upper limb is secured in the neutral position by the patient’s side padded with jelly cushions to protect potential pressure points. These patients are prepped with an aseptic solution and draped with legging drapes and an under-buttock drape followed by square draping to expose the entire anterior and lateral abdominal wall.
For creation of a transverse colostomy, and for the reversal of loop or double-barreled sigmoid colostomies, the patient is positioned supine, with the arms secured in the neutral position by the patient’s side padded with jelly cushions to protect potential pressure points (FIG 2B). For patients in the supine position, standard square draping is adequate.
Bladder decompression with a urinary catheter is not necessary except for closure of end sigmoid colostomy.
Gastric decompression with an orogastric tube, which is to be removed prior to completion of the general anesthetic, is used.
The laparoscopic equipment is assembled with all cords and tubes exiting/entering the sterile field over the right side of the patient’s chest.
All ports used are 5-mm balloon-tipped clear ports, with the exception of a 12-mm balloon-tipped port used through the stomal site.
We use a 5-mm 0-degree camera for insufflation-assisted optical entry into the peritoneal cavity and a 5-mm 30-degree camera at all other times.
Monopolar diathermy attached to laparoscopic scissors is adequate in almost all laparoscopic techniques described in this chapter. Advanced energy devices are reserved for difficult dissections and for the closure of end colostomies. For intracorporeal stapling and dividing, we use 60-mm reticulating linear endostaplers with 1.8-mm cartridge for division of colon and 1.2-mm cartridge for division of mesentery.
For extracorporeal stapling and dividing, we use 75-80 mm linear staplers with 1.8-mm closed staple height for colonic division, 1.5-mm closed staple height for the longitudinal staple line of double-stapled side-to-side anastomosis, and 1.8-mm closed staple height for the transverse staple line of double-stapled side-to-side anastomosis.
Five surgical team configurations are described in this chapter (FIG 3).
Configuration 1. The operating surgeon stands to the patient’s left side, with the surgical assistant to the patient’s right side and the instrument nurse adjacent to the patient’s right knee.
Configuration 2. The operating surgeon stands adjacent to the patient’s right side with his or her right hand dissecting with the energy device via the right lower quadrant (RLQ) or suprapubic (SP) port and with his or her left hand using a bowel grasper via right upper quadrant (RUQ) port. The assistant stands to the surgeon’s left side, with the camera in his or her right hand via the midline (ML) port and the bowel grasper via the stomal trephine (ST) or left lateral (LL) port site. The instrument nurse is adjacent to the patient’s right knee. The monitor is placed adjacent to patient’s left hip.
Configuration 3. The operating surgeon stands to the patient’s right side, with the dissecting energy device in his or her right hand via the ST or LL port and a bowel grasper in his or her left hand via the RUQ port. The assistant stands to the surgeon’s left side, with the camera in his or her right hand via ML port site. The instrument nurse or a second assistant stands between the patient’s lower limbs with a bowel grasper on his right or left hand via the RLQ port site. The monitor is placed adjacent to left side of the patient’s chest.
Configuration 4. The operating surgeon stands to the patient’s right side with the assistant to the patient’s left side and the instrument nurse adjacent to the patient’s right knee.
Configuration 5. The operating surgeon stands to the patient’s left side, with the dissecting energy device in his or her right hand via the LUQ port and the bowel grasper in his or her left hand via ST port (three-port transverse colostomy formation technique) or via the left lower quadrant (LLQ) port (four-port transverse colostomy formation technique). The assistant stands to the surgeon’s left side with the camera in his right hand via the ML port, and bowel grasper in his left hand via the ST port. The instrument nurse stands adjacent to the patient’s right knee. The monitor is placed adjacent to the right side of the patient’s chest.
Port placement planning and marking is important. The key to port placement is the RLQ port. The RLQ, RUQ, and ML ports should be placed a hand’s breadth distance from each other.
The RLQ port (5 mm) is inserted medial to, and at or just cranial to the level of the anterior superior iliac spine, just lateral to the path of the inferior epigastric vessels.
The RUQ port (5 mm) is inserted a hand’s breadth cranially along a craniocaudal line from the RLQ port.
The ML port (5 mm) is placed via a small incision in the umbilicus or supraumbilically in obese patients with pendulous abdomens.
The LL port (5 mm) is placed as laterally as possible at the level of the ML port. This port is optional, especially when the ST is created as the first step.
The ST port (5- or 12-mm) is placed at the preoperatively marked stoma site. If an endoscopic linear stapler is to be used, a 12-mm port is mandatory.
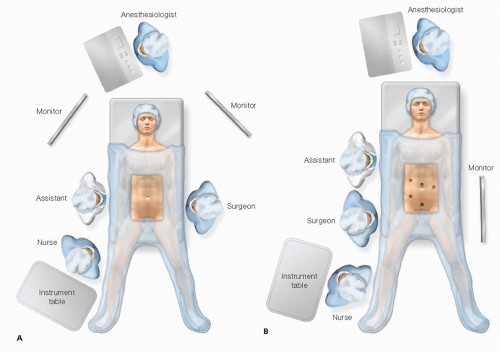 FIG 3 • Surgical team configuration and port placement. A. Configuration 1. B. Configuration 2. (Continued) |
When sure about the need of a colostomy, we prefer to create the ST as the first step before the contour and layers of the abdominal wall have been altered by a pneumoperitoneum or surgical incisions.
Using surgical team configuration 1 as previously described, a disc of skin at the preoperatively marked site is excised. Dissection through the subcutaneous adipose tissue proceeds to the anterior rectus sheath.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree