Laparoscopic Cholecystectomy and Common Bile Duct Exploration
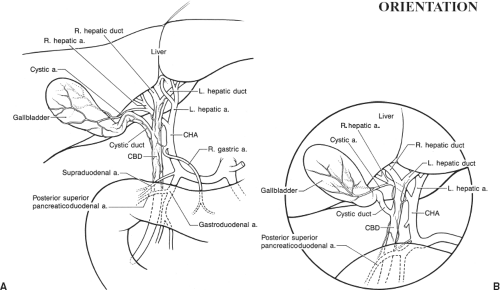
Laparoscopic cholecystectomy introduced operative laparoscopy to most general surgeons, and is often the first laparoscopic procedure performed by surgical residents. Although the anatomy is identical to that described in Chapter 72, the significance of some biliary anomalies is greater for the laparoscopic procedure. Accordingly, this chapter stresses not only surgical technique but also ways in which specific anatomic pitfalls can be avoided. It should be read in conjunction with Chapter 72. The regional anatomy is shown in Figure 73.1A with the more limited laparoscopic view demonstrated in Figure 73.1B.
This chapter describes the classic four-trocar approach. Many uncomplicated laparoscopic cholecystectomies are now done through a single incision approach, and natural orifice surgery (NOTES) has been adapted to this procedure as well. References at the end give details of these more advanced approaches.
SCORE™, the Surgical Council on Resident Education, classified laparoscopic cholecystectomy with and without cholangiography as “ESSENTIAL COMMON” procedures, and laparoscopic common duct exploration as a “COMPLEX” procedure.
STEPS IN PROCEDURES—LAPAROSCOPIC CHOLECYSTECTOMY
Obtain laparoscopic access and inspect abdomen
Place grasper on fundus of gallbladder and pull up and over the liver
Lyse any adhesions to omentum
Place second grasper on gallbladder infundibulum (Hartmann’s pouch)
Expose cystohepatic triangle
Incise peritoneum over distal gallbladder
Identify cystic duct and cystic artery
If cholangiogram is desired, insert catheter into cystic duct and secure it
Divide cystic duct and cystic artery
Dissect gallbladder from bed of liver, working in submucosal plane
Place gallbladder into retrieval bag and remove
Close trocar sites greater than 5 mm
HALLMARK ANATOMIC COMPLICATIONS—LAPAROSCOPIC CHOLECYSTECTOMY
Bile duct injury
Injury to duodenum
Injury to other surrounding viscera
Retained bile duct stone
LIST OF STRUCTURES
Bile Duct
Common hepatic duct
Right and left hepatic ducts
Cystic duct
Left and right subphrenic spaces
Subhepatic space
Lesser sac
Duodenum
Greater omentum
Hepatic artery
Cystic artery
Initial Exposure (Fig. 73.2)
Technical Points
Introduce the laparoscope through an umbilical portal. Place a 10-mm port in the epigastric region and two 5-mm ports in the right midclavicular line and right anterior axillary line (Fig. 73.2A). Explore the abdomen. Cautiously lyse any adhesions of gallbladder to colon, omentum, or duodenum (Fig. 73.2B). Pass a grasping forceps through the anterior axillary line port and grasp the fundus of the gallbladder, pulling it up and over the liver. This will expose the subhepatic space (Fig. 73.2C). If the stomach and duodenum are distended, have suction placed on an orogastric or nasogastric tube. Reverse Trendelenburg positioning and tilting the operating table right side up will help increase the working space by allowing the viscera to move caudad and to the left.
Place a second grasping forceps through the midclavicular line port and grasp Hartmann’s pouch. Pull out, away from the liver. This maneuver will open Calot’s triangle and create a safe working space (Fig. 73.2D).
Take a moment to orient yourself. Frequently, there is an obvious color difference between the pale blue or green of the gallbladder (unless severely diseased) and the yellow fat of the Calot’s triangle. This blue–yellow junction is a good place to begin dissection. A few filmy adhesions of omentum, transverse colon, or duodenum may need to be cautiously lysed to provide optimum visualization of the region. Calot’s node, often enlarged in acute or resolving acute cholecystitis, nestles in Calot’s triangle (Fig. 73.2E).
Another good landmark is the hepatic artery, which should be visible as a large pulsating vessel well to the left of the surgical field. This is a marker for the bile duct, which generally lies just to the right.
Anatomic Points
The cystic artery arises from the right hepatic artery in Calot’s triangle and ascends on the left side of the gallbladder in approximately 80% of individuals. A fatty stripe or slight tenting of the peritoneum overlying the gallbladder may serve as a clue to its probable location. In a significant minority of individuals, the cystic artery arises directly from the hepatic artery. Other anomalies of the cystic artery of laparoscopic significance are described in Figure 73.3.
Calot’s node is one of two fairly constant nodes in this region. The second node, termed the node of the anterior border of the epiploic foramen, lies along the upper part of the bile duct. Thus, simply noting the presence of a node in proximity to the bile duct does not guarantee a safe working distance from the bile duct.
Initial Dissection (Fig. 73.3)
Technical Points
Incise the peritoneum overlying the blue–yellow junction (Fig. 73.3A). The cystic duct should become evident as a tubular structure which runs into the gallbladder. It is generally
the closest structure to the laparoscope, and hence the first structure which is encountered. Develop a window behind the gallbladder by incising the gallbladder peritoneum on the left and right sides and blunt dissecting behind cystic duct and gallbladder (Fig. 73.3B). The cystic artery should be visible to the left of the cystic duct (Fig. 73.3C). With good traction outward on Hartmann’s pouch and an adequate peritoneal window, two tubular structures going to the gallbladder, the cystic duct and cystic artery, should be clearly seen (Fig. 73.3D).
the closest structure to the laparoscope, and hence the first structure which is encountered. Develop a window behind the gallbladder by incising the gallbladder peritoneum on the left and right sides and blunt dissecting behind cystic duct and gallbladder (Fig. 73.3B). The cystic artery should be visible to the left of the cystic duct (Fig. 73.3C). With good traction outward on Hartmann’s pouch and an adequate peritoneal window, two tubular structures going to the gallbladder, the cystic duct and cystic artery, should be clearly seen (Fig. 73.3D).
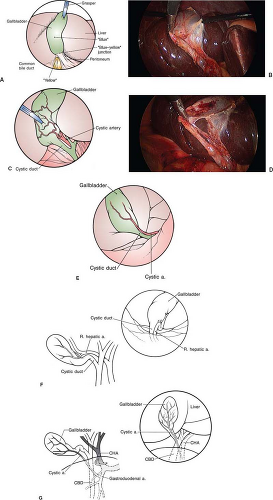 Figure 73.3 Initial dissection (A, C from Scott-Conner CEH, Brunson CD. Surgery and anesthesia. In: Embury SH, Hebbel RP, eds. Sickle Cell Disease: Basic Principles and Clinical Practice. New York, NY: Raven; 1994:809–827; B, D: Laparoscopic photographs kindly supplied by Evgeny V. Arshava, MD; E, F from Scott-Conner CEH, Hall TJ. Variant arterial anatomy in laparoscopic cholecystectomy. Am J Surg. 1992;163:590, with permission; G from: Cullen JJ, Scott-Conner CEH. Surgical anatomy of laparoscopic common duct exploration. In: Berci G, Cuschieri A, eds. Bile Ducts and Bile Duct Stones. Philadelphia, PA: WB Saunders; 1997:20–25, with permission).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|