Langerhans Cell Histiocytosis
Joseph Misdraji, MD
Key Facts
Etiology/Pathogenesis
Clonal proliferation of Langerhans dendritic cells
Clinical Issues
Affects infants and children
Multisystem LCH can involve “risk” organs: Liver, spleen, hematopoietic system
Permanent fibrosis of liver and lungs may occur, possibly due to “cytokine storm” produced by Langerhans cells
Results in secondary sclerosing cholangitis
Microscopic Pathology
Infiltration of liver by Langerhans cells, in small clusters or as a mass
Small duct infiltration and destruction, with features of chronic cholestasis and biliary fibrosis
Destructive cholangitis of large bile ducts with cystic dilatation and bile extravasation
Langerhans cells show abundant pink cytoplasm and lobulated nuclei, with fine chromatin
Langerhans cells often associated with eosinophils and other inflammatory cells, including non-Langerhans histiocytes
Ancillary Tests
Langerhans cells positive for S100, CD1a, and langerin
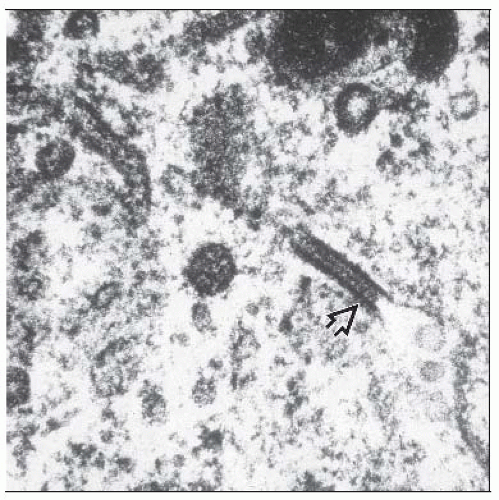
Electron microscopy shows Birbeck granules Diagnostic Checklist
LCH should be excluded in children with sclerosing cholangitis by staining for S100, CD1a, and langerin
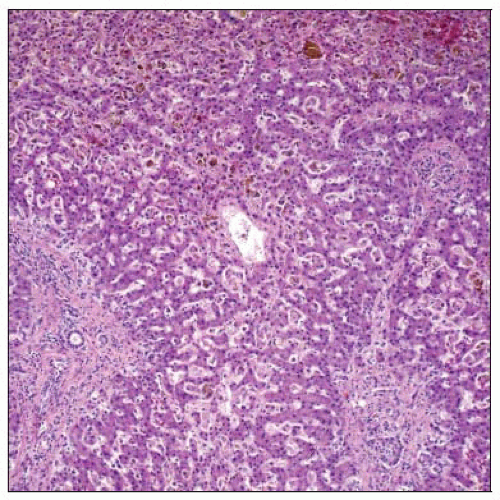 Langerhans cell histiocytosis in the liver features infiltration of the hepatic sinusoids by a mixture of Langerhans and non-Langerhans cells, with portal expansion and fibrosis. |
TERMINOLOGY
Abbreviations
Langerhans cell histiocytosis (LCH)
Synonyms
Histiocytosis X
Eosinophilic granuloma
Hans-Schüller-Christian disease
Letterer-Siwe disease
Definitions
Group of disorders characterized by clonal proliferation of Langerhans dendritic cells
ETIOLOGY/PATHOGENESIS
Clonal Disorder
Evidence of genetic aberrations favors neoplastic process
Loss of heterozygosity, chromosomal instability, elevated expression of cell-cycle-related proteins and oncogene products
CLINICAL ISSUES
Epidemiology
Incidence
Occurs in 4 per 1,000,000 children in United Kingdom of whom < 20% have hepatic involvement
Age
Infants and children, rarely adults
Site
LCH can involve single organ or multiple organs
Single-organ disease is most often bone or skin
Multisystem disease is subtyped according to involvement of “risk” organs
“Risk LCH” indicates involvement of liver, spleen, hematopoietic system
Presentation
Hepatosplenomegaly
Jaundice, cholestatic
Ascites
Hepatic dysfunction
Natural History
Permanent fibrosis of liver and lungs may occur, possibly due to “cytokine storm” produced by Langerhans cells
Results in pattern of sclerosing cholangitis
May progress to liver failure requiring transplantation
Treatment
Drugs
Etoposide, vinblastine, methotrexate
Prognosis
“Risk LCH” has 80% survival
Early therapy with nontoxic chemotherapy improves survival
Lack of response to chemotherapy at 6 weeks predicts poor survival
Reactivation usually occurs in nonrisk organs and is rarely fatal
IMAGE FINDINGS
Radiographic Findings
Endoscopic retrograde cholangiopancreatography (ERCP) shows strictures and beading of large intrahepatic and extrahepatic bile ducts, similar to primary sclerosing cholangitis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree