Kidney Needle Biopsy: Evaluation for Adequacy
SURGICAL/CLINICAL CONSIDERATION
Goal of Consultation
Determine if needle biopsy is adequate for a final diagnosis
Allocate tissue for special studies
Light microscopy (LM)
Immunofluorescence (IF)
Electron microscopy (EM)
Other studies depending on clinical situation
Culture for organisms
Tissue for molecular studies (e.g., tissue saved in fixatives such as RNAlater for RNA isolation)
Change in Patient Management
If specimen is deemed inadequate, additional needle biopsies will be taken
Clinical Setting
Medical renal biopsy
Generally performed for abnormal renal function or for urinary abnormalities
Should include renal cortex with glomeruli
Also performed to evaluate renal allografts
Allograft biopsies also benefit from IF and sometimes EM studies
Some centers perform surveillance (protocol) allograft biopsies at predetermined time points after transplant
Surveillance biopsies evaluate for subclinical rejection, viral infection, recurrent disease, etc.
Biopsies are usually performed under ultrasound guidance or CT guidance
Percutaneous (needle) biopsy
Ultrasound-guided, automated gun 16- to 18-gauge needle is usual
3 biopsy passes provide adequate sample (by Banff adequacy criteria) in 84% of cases in native and transplant biopsies
Compared to 18-gauge needle biopsies, 16-gauge needle biopsies provide more glomeruli & higher percentage of adequate biopsies with fewer passes
Transjugular renal biopsy may be performed in patients at high risk for bleeding (coagulopathy or thrombocytopenia)
Typically yields a smaller sample than percutaneous biopsy, but sufficient for diagnosis in > 90% of cases
Generally regarded as safe outpatient procedure
Hematuria may occur
Post-biopsy microscopic hematuria is usual
Gross hematuria in ˜ 3.5%
Other complications in 1-3% (varies with technique)
Higher risk of bleeding with 14-gauge needle biopsy; 16- and 18-gauge needle biopsies have a lower risk of bleeding
Perirenal hematoma ˜ 2.5%
Bleeding requiring transfusion in 0.9%
Hemorrhage requiring nephrectomy in 0.01%
Death in 0.02% (2 of 8,971 patients in a metaanalysis)
Intrarenal arteriovenous fistulas in ˜ 7% of allograft biopsies
Usually resolve
No apparent effect on renal function
Page kidney (described by Dr. Irwin Page)
Most commonly due to trauma, but rare cases occur due to bleeding after kidney biopsy
Compression of kidney by accumulation of blood in perinephric or subcapsular space
Usually manifests with renin-dependent reactive hypertension due to renal ischemia, occasionally presents with renal insufficiency
SPECIMEN EVALUATION
Gross
Biopsies must only be touched by clean forceps
Minute amounts of formalin can alter antigenicity of tissue used for immunofluorescence
Glutaraldehyde contamination can complicate interpretation by light microscopy and on immunoperoxidase stains
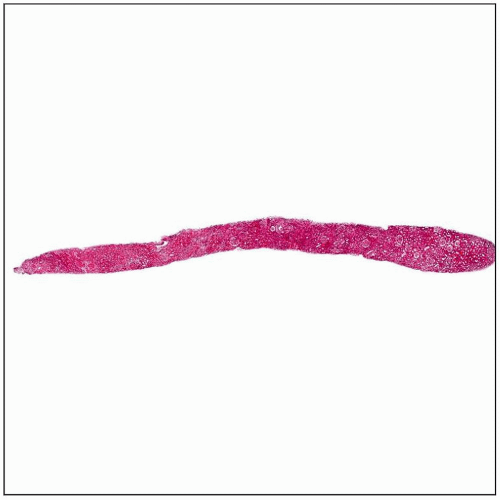
Needle biopsies are best examined under stereomicroscopy (dissecting microscope)
If dissecting microscope is not available, renal biopsies can be examined using magnifying glass
For evaluation of allografts, ≥ 10 glomeruli and 2 arteries must be present (Banff criteria)
Glomeruli are pink to red nodules (“raspberries”) in a pale tan background
Allocation of Tissue
In majority of cases, tissue is saved for light microscopy, IF, and EM
Appropriate allocation of tissue depends on several factors
Clinical differential diagnosis
Focality of expected disease
Amount of tissue available
Light microscopy
Tissue is fixed in formalin
Standard histochemical stains are H&E, PAS, Jonesmethenamine silver, and trichrome
Additional stains ordered depending on clinical setting and light microscopy appearance
Immunofluorescence
Cortex and medulla are placed in Zeus transport solution (Michel solution)
Standard immunohistochemical studies are IgA, IgG, IgM, kappa, lambda, C3, C1q, albumin, and fibrin
C4d is added for allograft biopsies to evaluate for antibody-mediated rejection
If no glomeruli are present in tissue submitted in Zeus medium, IF staining may still be contributory
Detection of monoclonal immunoglobulin deposition disease, light chain cast nephropathy, AL or AH amyloidosis, etc.
C4d staining of peritubular capillaries for transplant biopsies (C4d may also be performed by immunoperoxidase staining)
If no glomeruli present in frozen IF tissue, IF can be performed on pronase-digested paraffin sections
Pronase-digested paraffin IF less sensitive than routine IF on frozen tissue
Electron microscopy
Tissue with a few glomeruli are saved in Karnovsky glutaraldehyde/paraformaldehyde fixative
If limited tissue, tissue processed for light microscopy can be deparaffinized for electron microscopy
This technique shows some artifacts that can inhibit interpretation
Artifactual glomerular basement membrane thinning does not allow for diagnosis of thin glomerular basement membrane nephropathy on deparaffinized samples
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree