Isolated Limb Perfusion
Omgo E. Nieweg
Oscar E. Imhof
Bin B.R. Kroon
DEFINITION
Compared to other cancer types, melanoma has a particular biology in various respects. In-transit dissemination is typical of this disease and occurs in a few percentage of patients. In-transit metastases grow from tumor cells that are stuck in a lymph vessel in the skin or in the subcutaneous tissue. Such metastases are preferably excised but they tend to recur in larger numbers (FIG 1). Isolated perfusion can be considered when they are situated on a limb and their number is too great or they recur too frequently.
Isolated limb perfusion (ILP) enables treatment of an arm or leg with a high dose of chemotherapy without exposing the remainder of the body to the drug(s). This is accomplished by isolating the limb from the body’s circulation and creating a separate oxygenated blood circuit. This is in contrast to isolated limb infusion (ILI), a low-flow, nonoxygenated perfusion that is described in Part 5, Chapter 33. ILP and ILI are therapeutic options for patients with locally or regionally advanced melanoma that would otherwise require a more debilitating operation, for example, amputation.
PATIENT HISTORY AND PHYSICAL FINDINGS
After treatment of their primary melanoma, patients are instructed to regularly examine the scar of the excision for local recurrence and to check the skin and subcutaneous tissue around this area up to the regional lymph node basin for visible or palpable satellite and in-transit metastases. The physician who follows the patient inquires about new regional lesions. Patients themselves detect about half of the recurrences, but at an early stage, they can look quite innocuous. The detection of the more subtle ones requires the expertise and suspicious mind of an experienced surgeon.
A detailed history should be obtained to assess the general condition of the patient and to be informed about other relevant ailments, allergies, and medication.
Physical examination of melanoma patients is aimed at detecting a local recurrence, satellite metastases, in-transit metastases, regional lymph node involvement, and a subsequent primary melanoma. A detailed examination of the skin, the regional subcutaneous tissue, and the regional node field is warranted.
The vascular situation of the limb is assessed. The presence of peripheral arterial pulsations needs to be sufficient to allow for ILP.
IMAGING AND OTHER DIAGNOSTIC STUDIES
The presence of advanced melanoma in the extremity should be confirmed by biopsy.
In addition to the routine preoperative tests, screening for metastases elsewhere is appropriate as their presence may change the treatment plan. Whole body positron emission tomography (PET) or computed tomography (CT) and magnetic resonance imaging (MRI) of the brain are frequently recommended for this purpose.
Arteriography is indicated if the arterial blood supply is questionable. A complete obstruction in the target artery or a major impediment downstream renders perfusion impossible. Extensive arterial calcification per se is not a contraindication.
An elevated tumor marker such as the TA90 glycoprotein antigen or the S100 protein provides an opportunity to monitor the course of the disease.
SURGICAL MANAGEMENT
Rationale and Contraindications
Extensive involvement limited to a certain region is typical for melanoma.
The rationale for ILP is that melanoma is sensitive to cytotoxic drugs but effective treatment requires a higher dosage compared to various other cancer types. In contrast to the vital organs, the normal tissues in the extremities tolerate such a high dose. ILP with cytotoxic medication may improve regional tumor control while limiting the systemic side effects.
The procedure makes it possible to vary physiologic conditions such as blood flow, temperature, and oxygenation.
Prophylactic ILP is not indicated in patients with excised high-risk primary melanoma without evidence of regional metastases.1
The contraindications are listed in Table 1. A major vascular obstruction may prevent access to the artery and precludes the operation.
Diabetes mellitus with severe peripheral vascular disease is a contraindication.
ILP should not be performed in children as it may damage the epiphyseal plates.
Previous radiotherapy is a relative contraindication as perfusion may cause necrosis of prior irradiated skin.
A large superficial tumor with major tendon involvement is a relative contraindication.
Table 1: Absolute and Relative Contraindications to Isolated Limb Perfusion
Absolute contraindications
Obstruction of major artery
Diabetes with serious peripheral vascular disease
Child with open epiphyseal plates
Relative contraindications
Previous radiotherapy
Large superficial tumor with major tendon involvement
Brain metastases
Infected wound or ulcer
Brain metastases tend to bleed and their presence is a relative contraindication.
An infected wound or ulcer is another relative contraindication.
ILP can be carried out safely at an advanced age.2 The presence of regional node involvement is not a contraindication, as this procedure can be combined with a regional node dissection. In the presence of distant metastases, systemic therapy is a reasonable first option, but perfusion can provide good regional palliation in the presence of refractory bloodborne metastases.
Anatomy
For advanced disease of the leg, ILP can be performed at the femoral or iliac level. The arm can be treated at the brachial level or through the axilla.
Preoperative Planning
ILP requires cooperation of the surgeon, the perfusionist, and the nuclear medicine worker in addition to the customary operating room team.
Melphalan is the standard drug used in current practice. The dosage of the drug is adjusted to the need of the individual patient. The volume of the extremity is an often used parameter to calculate the required melphalan dose. The volume can be determined using a water reservoir (FIG 2). Adjustments to the dosage can be made based on risk factors for regional toxicity like female gender and obesity.
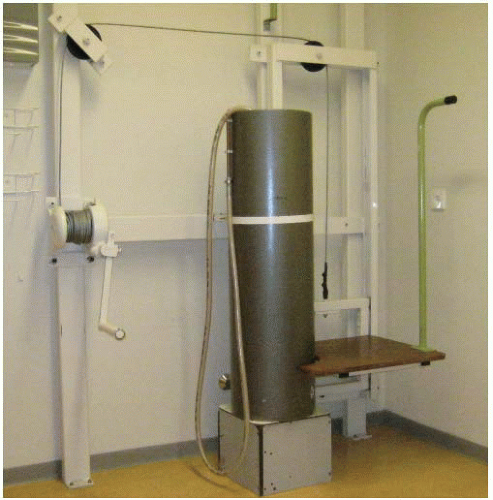
FIG 2 • Water reservoir for measuring the volume of a limb. On the right is the elevator to bring the patient up to the required height. The elevator handle is on the left.
ILP requires sophisticated technology. The surgeon should verify the availability of the required drug(s) and make sure that the necessary equipment and materials are present and in good working order.
General anesthesia is required. Epidural anesthesia is to be avoided as it induces vasodilation and predisposes to leakage of blood from the systemic circulation to the perfusion circuit.
Preoperative antibiotics are not necessary.
TECHNIQUES
ISOLATED FEMORAL PERFUSION
Positioning
The patient is placed on the operating table in a supine position. The leg may be slightly exorotated.
The leg is prepped and draped in a sterile fashion in its entirety.
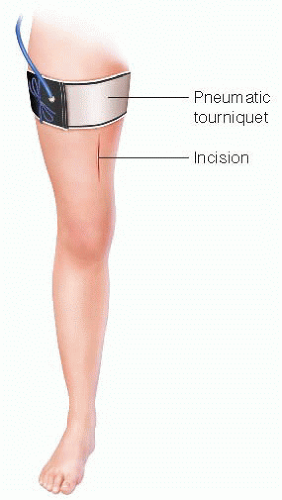
A pneumatic tourniquet is positioned around the upper thigh, but it is not inflated yet.
A heating blanket is wrapped around the knee and the lower leg.
A cotton doughnut is positioned underneath the heel to prevent decubitus.
The operating table is tilted toward the surgeon.
Incision
Access to the Superficial Femoral Vessels and Cannulation
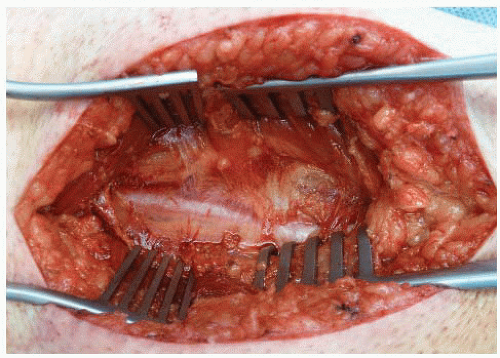
The external femoral vessels run behind the sartorius muscle. The vessels are reached either medially or laterally from the muscle. The thin fascia covering the vessels (FIG 5) is incised, exposing the superficial femoral artery. The artery is mobilized over the exposed length (FIG 6). Small arteries branching from the superficial femoral artery are ligated and divided. A vessel loop facilitates the dissection. The accompanying vein is identified when the artery is pulled aside (FIG 7). The vein is mobilized over the exposed length. Attributing branches are ligated at the confluence and divided.
Heparin is administered in a quantity of 150 units/kg body weight.
Open access to the saphenous vein at the level of the ankle is gained to measure the venous pressure. The venous pressure is monitored throughout the procedure and should not deviate more than 10 mm H2O from the initial assessment. An increase is associated with postoperative morbidity.
The appropriate diameter of arterial and venous cannulae for the perfusion is determined. The cannulae are tunneled subcutaneously underneath the tourniquet to the open wound to prevent kinking.
The vein is clamped cranially and caudally. A transverse venotomy of a few millimeters is performed. The cannula is inserted caudally and secured with the vessel loop (FIG 8A,B). The cannula is hooked up to the extracorporeal circuit and 300 mL of blood is tapped for the perfusion circuit. Subsequently, the arteriotomy is performed in a similar fashion and the arterial cannula is introduced and secured, and the circuit is completed (FIG 9).
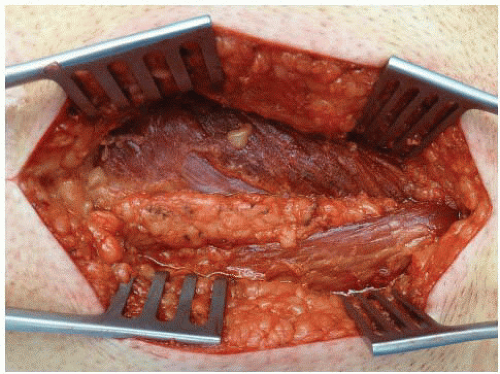 FIG 4 • The long adductor muscle (above) and the sartorius muscle (below) are exposed. The superficial femoral vessels lie behind the sartorius muscle. |
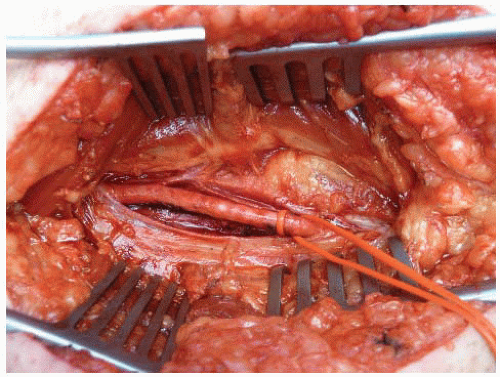 FIG 6 • The superficial femoral artery is mobilized.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|