Isolated Limb Infusion
Jeffrey J. Sussman
Joseph S. Giglia
DEFINITION
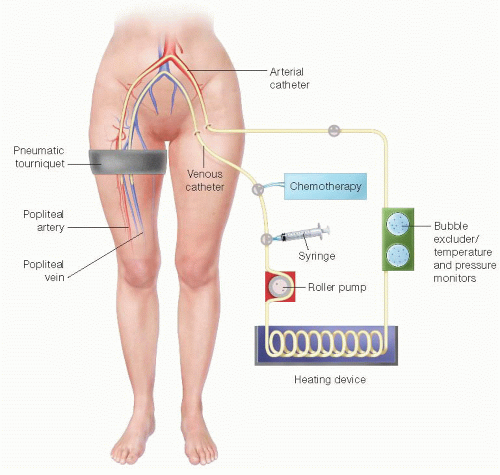
Isolated limb infusion is the term that is commonly used to indicate a minimally invasive, low flow rate, nonoxygenated perfusion of an extremity with chemotherapy to effect control of a cancer within that extremity1 (FIG 1). It is a more recent modification of a more traditional technique commonly referred to as isolated limb perfusion (see Part 5, Chapter 34), which uses higher flow rates and an oxygenated circuit to perfuse the chemotherapy through the extremity where vascular control is obtained during an open procedure and is often combined with a formal node dissection. Comparatively, isolated limb infusion is a shorter, better tolerated, less complex procedure, not requiring a perfusionist, an oxygenator, nor blood products to prime the extracorporeal circuit.2,3 Proponents of limb perfusion claim a higher response rate, particularly in bulky disease; however, the techniques have not been compared in a randomized fashion.
PATIENT HISTORY AND PHYSICAL FINDINGS
The most common indication for this procedure is a patient with in-transit melanoma restricted to an extremity whose lesions are too numerous or recurrent to be amenable to simple excision. It should be thought of as a limb salvage technique to treat regionally advanced disease and has no proven systemic benefit. Therefore, it is not commonly used in the face of distant metastasis unless regional control/palliation is the central goal.
Common malignancies treated in this manner include melanoma and Merkel cell carcinoma. Other histologies treated less commonly include squamous cell carcinoma and sarcoma.
A through history and physical should be performed with attention to documenting location and extent of extremity disease, limb function, edema, vascular exam, and evaluation of draining nodal basins.
Limb volume is estimated by water displacement.
Sequential circumferential measurements or computed tomography (CT) volumetric measurements have been described as alternatives.
The contralateral limb should be measured if the involved limb is edematous.
The limb is submerged in a water tank up to level anticipated to be at bottom of tourniquet. The water level is marked and then after removal of the limb, the tank is filled with a measured amount of water to reach the marked level.
Patients should have nonoccluded arterial and venous systems to allow catheter placement and chemotherapy infusion.
The extent of disease needs to be distal enough in the extremity to be able to place a tourniquet proximally.
In selected cases, this may require resection of limited more proximal disease combined with infusion of greater distal disease burden distally.
Isolated limb infusion can be combined with a lymph node dissection with direct placement of the catheters in the exposed vessels.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Arterial and venous duplex ultrasound to establish arterial and venous patency. With adequate collaterals, limb infusion has been described even when superficial vessels are occluded.
Imaging to evaluate limb disease burden if lesions are deep seated and difficult to quantitate on exam
Imaging to evaluate for distant disease including brain magnetic resonance imaging (MRI); whole body positron emission tomography (PET)/CT; and/or chest, abdomen, pelvis contrast-enhanced CT scans
SURGICAL MANAGEMENT
Patients should be discussed in multidisciplinary fashion to consider alternatives to isolated infusion including isolated limb perfusion; intralesional therapy; simple excision; radical excision, including circumferential excision and grafting or amputation; radiation; or systemic cytotoxic, immunotherapeutic, and other biologic therapies as well as clinical trial eligibility.
Preoperative Planning
Who and where vascular access is to be obtained should be determined preoperatively and may be institution specific. Possible methods include the following:
Interventional radiology. Vascular access can be performed in the interventional radiology suite, with the patient then transported to the operating room (OR) with the arterial and venous catheters in place.
Vascular surgery. Some vascular surgeons have the training, experience, and interest to perform the vascular access as an alternative to the interventional radiologist. Access can be obtained in the OR directly if appropriately equipped with fluoroscopic capabilities. Although additional OR time is required if done in the OR, the catheters can more easily be manipulated later, as needed. Moreover, access can be obtained under general anesthesia and risk of dislodgement during transport/bed transfer is eliminated.
Chemotherapy. Melphalan and dactinomycin are prepared just prior to the procedure. The calculated drug dosage is often reduced if the patient’s actual body weight exceeds ideal body weight by multiplying the calculated drug dose by the ratio of ideal to actual body weight.
Melphalan dose is 7.5 mg/L volume for lower extremity infusions (maximum dose of 100 mg) or 10 mg/L volume for the upper extremity (maximum dose 50 mg).
Dactinomycin dose is 1% of the melphalan dose (maximum 0.5 mg).
The drugs are mixed together in 400-mL normal saline lower extremity (200 mL upper extremity) and delivered to OR for administration.
Positioning
The patient is positioned supine on a fluoroscopy-capable OR bed for vascular access or in case catheter manipulation is needed.
The room should be prewarmed.
A heated circulating water blanket is placed around the affected extremity or an external radiant heater utilized (FIGS 2 and 3).

FIG 3 • Affected limb wrapped in water blanket.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access