Internal Mammary Sentinel Node Biopsy
A. Marilyn Leitch
DEFINITION
Internal mammary node dissection is performed for both diagnostic and therapeutic purposes. This surgery is generally performed in conjunction with breast cancer surgery as part of nodal staging. In modern times, this usually involves removal of lymph nodes from one or two parasternal interspaces as part of a sentinel node staging procedure. In the first descriptions of internal mammary node dissection, the entire internal mammary nodal chain was resected including the adjacent ribs.1 With the advent of sentinel lymph node mapping, it is possible to perform a more minimally invasive procedure to resect in a directed fashion internal mammary nodes that are demonstrated to have lymphatic drainage from the breast. Internal mammary sentinel node drainage is identified on lymphoscintigraphy in 10% to 22% of mapping studies. Internal mammary drainage is more likely to be identified if the radionucleotide is injected in the peritumoral region rather than subareolar. The technique described here to retrieve sentinel nodes can also be used to surgically biopsy small suspicious internal mammary nodes identified on preoperative imaging with computed tomography (CT) scan or breast magnetic resonance imaging (MRI).
PATIENT HISTORY AND PHYSICAL FINDINGS
The breast cancer patient should have a careful evaluation with a complete history and physical examination as well as appropriate imaging studies. The patient’s history should focus on specific breast complaints including how long the patient has been aware of the cancer in her breast, associated symptoms and signs, and focal chest wall pain. It is important to ascertain the patient’s medical history to assess the patient’s risk for surgery related to intercurrent medical conditions. Prior surgery such as sternotomy, coronary artery bypass graft, thoracotomy, and breast augmentation should be noted, as these may complicate the performance of internal mammary node dissection. Past history should include annotations about prior radiation to the chest wall such as mantle radiation for Hodgkin’s disease. The patient should be queried about prior trauma to the anterior chest wall.
Physical examination includes the full examination of the breast to document any palpable mass lesion, including the size and location with respect to the quadrant of the breast and its distance from the nipple. The nodal basin should be carefully examined including the cervical, supraclavicular, axillary basins, as well as the palpation of the parasternal region. If there are any evident abnormal nodes, these should be further evaluated with imaging including mammography and ultrasound. Needle biopsy of suspicious nodes can be undertaken preoperatively in order to plan the therapeutic intervention.
IMAGING AND OTHER DIAGNOSTIC STUDIES
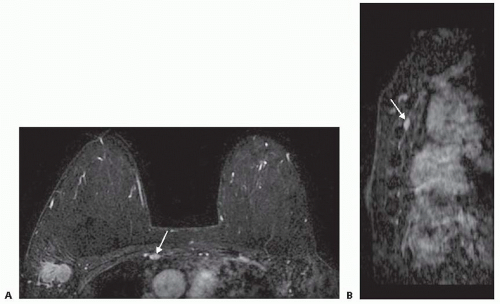
The standard imaging workup for a newly diagnosed breast cancer patient would include mammography and ultrasound of the breasts. Many patients will have an MRI performed as well. This study permits visualization of the internal mammary nodal chain. If an abnormal lymph node is identified, it can be biopsied with a needle or targeted for excision at the time of surgery (FIG 1A,B).
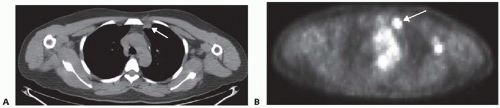
CT scanning of the chest is not routine for the workup of that early-stage breast cancer. However, if a CT scan of the chest or positron emission tomography (PET)-CT is performed for other indications, internal mammary node enlargement may be identified (FIG 2A,B). If the patient has palpable fullness in the parasternal region, a CT scan should be ordered to evaluate for internal mammary nodal metastases.
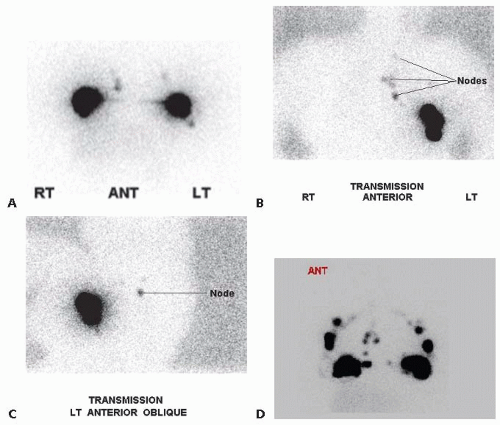
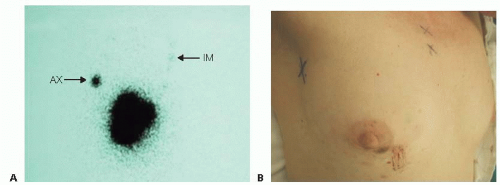
In order to identify the internal mammary nodal drainage in the sentinel node procedure, it is critical to inject a radiolabeled tracer for mapping of the pathways to the internal mammary nodes. To maximize the chance of identifying internal mammary lymphatic drainage, it is important to perform the injections of technetium sulfur colloid in the peritumoral region rather than performing a subareolar injection only. Lymphoscintigraphy can be performed to have a visual representation of the location of the internal mammary drainage (FIG 3A-D). The area of radioactivity in the parasternal region can be marked on the skin by the nuclear medicine technician at the time of scanning (FIG 4A,B). This increases the efficiency of identifying the appropriate interspace for exploration for the sentinel node. Most commonly, there will be one interspace that demonstrates a hot spot. However, more than one interspace may demonstrate a radioactive focus. The most common areas of drainage are the 2nd and 3rd interspaces.
SURGICAL MANAGEMENT
Preoperative Planning
The lymphoscintigraphy should be reviewed prior to going into the operating room. It is important to consent the patient specifically for the internal mammary exploration. Knowing from the lymphoscintigraphy that there is internal mammary lymphatic drainage, the surgeon can convey to the patient that this pathway can be pursued if the patient is agreeable. If it is the practice of the surgeon not to perform lymphoscintigraphy prior to surgery, then the interspaces can be examined intraoperatively with the gamma probe to identify foci of increased radioactivity in the parasternal interspaces. It remains important to consent the patient for the possibility of an internal mammary exploration with its potential complications.
Positioning
The patient is positioned supine with the arms abducted to 90 degrees on padded arm boards. The skin prep of the chest wall should cross to the contralateral breast so that the sternum and parasternal regions are draped into the field of operation.
TECHNIQUES
INCISION AND INITIAL IDENTIFICATION OF AREA OF INTERNAL MAMMARY SENTINEL NODE
Placement of the incision is governed by the procedure planned for resection of the breast tumor. For patients having breast-conserving surgery, the incision for the primary tumor is placed overlying the primary lesion. If the primary lesion is near to the area of internal mammary drainage, then it may be feasible to explore the interspaces via the partial mastectomy incision. However, if the primary lesion is distant from the parasternal region, then the incision for exploration of the interspace is placed overlying the area of focal radioactivity.
If the patient is undergoing a mastectomy, the standard mastectomy incision is used for accessing the parasternal interspaces (FIG 5). When reconstruction is planned, the mastectomy incision is generally more limited with the skin-sparing technique. However, the parasternal region can be generally accessed via these incisions with retraction of skin flaps, unless there is nipple preservation with the incision placed in the inframammary line. In this circumstance, the incision location would be determined in a similar fashion as patients having breast-conserving surgery.
It is much easier to identify the area of focal radioactivity in the interspaces after the breast is removed or after the partial mastectomy is completed. This reduces the amount of background radioactivity, which increases the ease of identifying radioactivity in an internal mammary node. In order to find an internal mammary sentinel node, it is imperative to have a strong signal that can be picked up by the gamma probe to direct the incision placement.
Lymphazurin blue, which is often injected for identification of the sentinel nodes in the axilla, should be injected prior to beginning any resective procedure in the operating room. Lymphazurin blue alone will not be successful in identifying the internal mammary sentinel nodes. However, once the area of radioactivity is identified and exploration is begun, blue lymphatics or staining of the sentinel nodes may be identified but not with the frequency that it is seen in the axillary nodes. As with the radioactive tracer, the blue dye is more likely to be identified in the internal mammary nodes if the injection is peritumoral.
After the blue dye is injected, the axillary sentinel node exploration is then begun. (Refer to Part 5, Chapter 8 for more information on sentinel node dissection.) In most cases, there will be an axillary sentinel node identified in those patients who also have internal mammary drainage.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree