Internal Drainage of Pancreatic Pseudocysts
Pancreatic pseudocysts form when collections of fluid become loculated in the region of the pancreas and fail to reabsorb, becoming chronic. The term “pseudocyst” reflects the lack of a true internal cyst lining. Most pancreatic pseudocysts are found in a retrogastric location in the lesser sac. Many of these collections are now managed by percutaneous or endoscopic drainage (see references at the back). Surgery is reserved for chronic refractory pseudocysts.
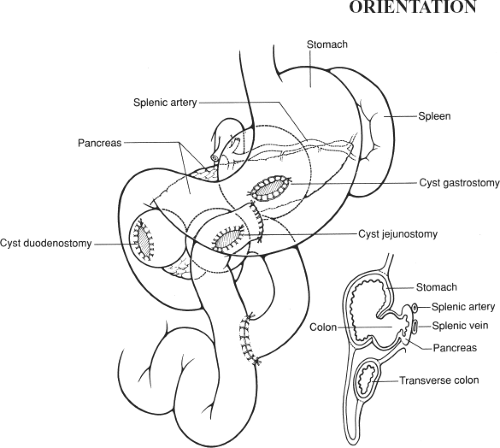
Proximity to the back wall of the stomach makes internal drainage by cyst gastrostomy the procedure of choice. Occasionally, a pseudocyst in the head of the pancreas may require drainage by anastomosis to the duodenum (cyst duodenostomy); in other cases, a very dependent pseudocyst that is not close to the back wall of the stomach may require drainage by Roux-en-Y cyst jejunostomy. These procedures are illustrated schematically in Figure 86.1, which also shows the relative regional anatomy.
SCORE™, the Surgical Council on Resident Education, classified drainage of pancreatic pseudocyst as an “ESSENTIAL UNCOMMON” procedure.
STEPS IN PROCEDURE—CYST GASTROSTOMY
Upper midline or chevron incision
Explore abdomen
Confirm retrogastric location
Place two stay sutures on anterior surface of stomach, centered on cyst
Create longitudinal gastrotomy
Aspirate Cyst Through Posterior Wall of Stomach (Check for Blood)
Full-thickness biopsy of cyst wall
Oversew edge of cystogastrostomy with running lockstitch
Check hemostasis
Close gastrotomy and cover with omentum
Close abdomen without drains
HALLMARK ANATOMIC COMPLICATIONS—CYST GASTROSTOMY
Premature closure with recurrence of cyst
Bleeding
LIST OF STRUCTURES
Pancreas
Head
Body
Tail
Uncinate process
Spleen
Splenic artery
Splenic vein
Colon
Transverse mesocolon
Middle colic artery and vein
Stomach
Greater curvature
Pylorus
Antrum
Duodenum
First and second portions
Bile duct
Left and right gastroepiploic arteries and veins
Gastrocolic omentum
Gastropancreatic folds
Gastroduodenal artery
Inferior vena cava
Cyst Gastrostomy
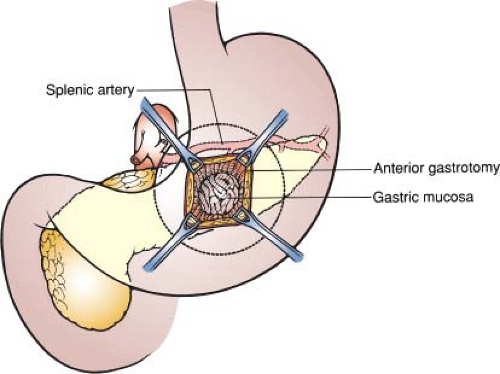
Delineation of Anatomy and Preparation for Anastomosis (Fig. 86.2)
Technical Points
Use an incision that provides good exposure to the epigastric region. Generally, an upper midline or a chevron-type incision, depending on the build of the patient, is elected. Palpate the abdomen after the patient is asleep and plan an incision that is located directly over the palpable mass, if possible.
The typical retrogastric cyst is approached through the anterior wall of the stomach. Place stay sutures of 2-0 silk in the anterior wall of the stomach in a convenient and mobile location, well away from the pylorus. Incise the gastric wall longitudinally with electrocautery. A generous longitudinal gastrotomy, at least 5 to 6 cm in length, is needed. Secure all bleeding points. Place an 18-gauge needle into the pseudocyst through the posterior wall of the stomach. Aspirate and confirm that there is no blood in the cyst. If blood is obtained on aspiration, the possibility of a cyst eroding into the splenic artery should be strongly considered. (In this case, consider closing the abdomen and obtaining angiographic embolization.) Alternatively, the cyst must be widely opened through the gastrocolic omentum and direct suture control of the splenic artery achieved. Splenectomy may be needed. Closed-suction drains must then be placed in the cyst to provide external drainage. Culture the cyst fluid.
Aspirate about 100 mL of cyst fluid and then inject 50 to 100 mL of water-soluble contrast material and obtain a radiograph. This will demonstrate the anatomy of the cyst and whether or not there are septations that must be treated. Depending on the adequacy of preoperative studies, this step may be omitted. Place stay sutures in the posterior gastric wall and prepare to make an incision into the back wall of the stomach.
Anatomic Points
The anatomic relationships of the pancreas, the location of the pancreatic pseudocyst, and the anatomic fusion of adjacent organs in response to inflammation allow internal drainage of pancreatic pseudocysts.
The head of the pancreas lies in the duodenal curve. Superiorly, it is overlapped anteriorly by the first part of the duodenum; elsewhere, its margin is indented by the duodenum. Its anterior anatomic relationships include the first part of the duodenum, the gastroduodenal artery (which makes a groove in the pancreas that delineates head from neck), the transverse mesocolon, and the jejunum. Posteriorly, the head of the pancreas lies on the right diaphragmatic crus, the inferior vena cava and terminal segments of the renal veins, and the aorta. The inferior part of the head is continuous with the uncinate process, which lies in the space between the superior mesenteric vessels and the aorta. The bile duct is either posterior to the head of the pancreas or embedded within the substance of this gland.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree