Inflammatory Myofibroblastic Tumor
Karen S. Thompson, MD
Key Facts
Terminology
Tumor of myofibroblastic spindle cells with inflammatory infiltrate of plasma cells, lymphocytes, and eosinophils
Intermediate biological potential: Propensity to recur, but metastases are rare
Clinical Issues
Most common sites include lung, mesentery, and omentum
1/3 of patients present with clinical syndrome including
Fever, malaise, growth failure, weight loss, anemia, thrombocytosis, polyclonal hyperglobulinemia, elevated ESR
Prognosis is difficult to predict based on histopathology alone
Increased aggressive potential: Aneuploidy, p53 positivity, cytologic atypia
Microscopic Pathology
3 histologic patterns
Loosely arranged plump myofibroblasts
Compact spindle cells in fascicles
Low cellularity scar-like pattern
Immunohistochemical positivity for ALK not specific for IMT but positive in 50% of cases
Ancillary Tests
50-70% of IMTs are positive for ALK gene rearrangements involving 2p23
TERMINOLOGY
Abbreviations
Inflammatory myofibroblastic tumor (IMT)
Synonyms
Inflammatory pseudotumor, plasma cell granuloma, plasma cell pseudotumor, pseudosarcomatous myofibroblastic lesion
Definitions
Lesion of myofibroblastic spindle cells with inflammatory infiltrate of plasma cells, lymphocytes, and eosinophils
Intermediate biological potential
Unknown etiology
Term inflammatory pseudotumor has been used to describe multiple different entities, thus its use is discouraged
ETIOLOGY/PATHOGENESIS
Anaplastic Lymphoma Kinase (ALK) Mutations
Many IMTs have clonal rearrangement of ALK gene thought to be a key event in its pathogenesis, which supports current view of this tumor as true neoplasm
Mutation results in expression and activation of ALK gene
Various fusion partners have been described, which explains the different patterns of ALK protein immunoreactivity
CLINICAL ISSUES
Epidemiology
Age
Occurs most commonly in children and young adults; average age: 10 years
Gender
Slight female predominance
Presentation
Visceral and soft tissue tumor
Most common sites
Lung, mesentery, omentum, and gastrointestinal tract
Other sites
Soft tissue and bladder
Presenting symptoms related to anatomic location of tumor
Pulmonary IMT can present with chest pain and dyspnea
Abdominal IMT can present with gastrointestinal obstruction
May also be asymptomatic with discovery as incidental finding during work-up for unrelated disease or symptom
Clinical syndrome in 1/3 of patients
B symptoms
Fever, growth failure, malaise, weight loss
Anemia
Thrombocytosis
Polyclonal hyperglobulinemia
Elevated erythrocyte sedimentation rate (ESR)
Syndrome resolves with excision of mass
Treatment
Complete surgical resection is preferred treatment modality
Chemotherapy, steroids, and nonsteroidal anti-inflammatory drugs (NSAIDs) have been tried as adjunctive therapies with variable success
May be tried in aggressive or metastatic disease
Prognosis
Difficult to predict based on histopathology alone
Vast majority behave in benign fashion
Increased aggressive potential associated with the following
Aneuploidy
Expression of p53
Cytologic atypia
Recurrence rates
ALK gene rearrangements associated with younger age and higher recurrence rates
Pulmonary tumors confined to lung (1.5%)
Extrapulmonary tumors confined to a single organ (8%)
IMTs found outside a single organ at presentation (35%)
Abdominal IMTs (33%)
Metastases are rare
IMAGE FINDINGS
Radiographic Findings
Lobulated solid mass with or without calcifications
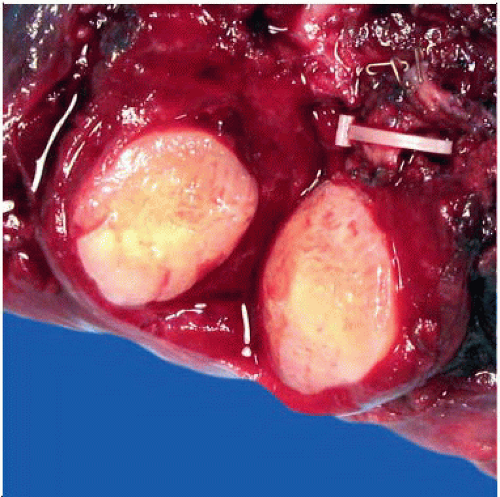
MACROSCOPIC FEATURES
General Features
Circumscribed, solitary or multinodular mass
Firm, rubbery, tan-yellow, white or gray fleshy cut surface
Focal hemorrhage, necrosis, and calcifications in some cases
6 cm in average diameter, reported range 1-22 cm
Most tumors are 5-10 cm in diameter
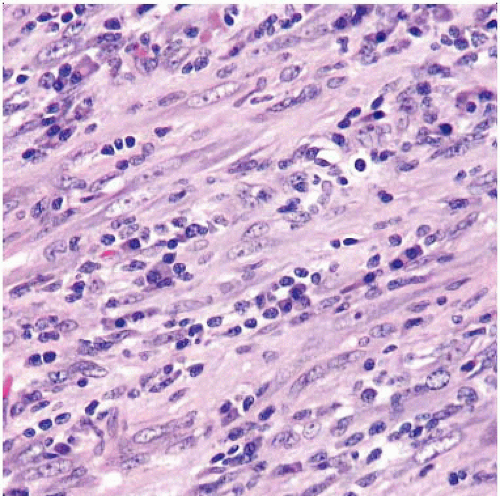
MICROSCOPIC PATHOLOGY
Histologic Features
3 histologic patterns, all of which may intermingle within a single tumor
Loosely arranged plump myofibroblasts, “nodular fasciitis-like”
Edematous myxoid background
Mixed infiltrate of plasma cells, lymphocytes, and eosinophils
Ganglion-like myofibroblasts
Numerous blood vessels
Extravasated red blood cells infrequently seen
Compact spindle cells with storiform or fascicular growth pattern
Variable myxoid and collagenized regions
Mixed infiltrate of plasma cells, lymphocytes, and eosinophils
Small aggregates of plasma cells or lymphoid nodules
Ganglion-like myofibroblasts
Low cellularity scar-like pattern
Plate-like collagen
Sparse inflammation with plasma cells and eosinophils
Osseous metaplasia or calcifications may be present
Collections of foam cells are seen in some cases
Mitoses may be present but are not atypical
Many tumors have large amounts of plasma cells (thus old name of plasma cell granuloma) and lymphocytes
Histologic evolution to a higher grade
Does not necessarily predict aggressive behavior or metastases
Highly atypical polygonal cells
Oval vesicular nuclei with prominent nucleoli
Variable mitoses, some of which may be atypical
Large ganglion-like cells
Reed-Sternberg-like cells
Associated with p53 immunoreactivity
ANCILLARY TESTS
Molecular Genetics
50-70% of IMTs are positive for ALK gene rearrangements involving chromosome 2p23
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree