History of Therapeutic Approaches to Acid Related Diseases
The evolution of therapy
|
Prout initially identified gastric acid as hydrochloric acid in 1823. However, it was only in the late nineteenth century that hyperchlorhydria was recognized as contributing to ulcer generation. For centuries, treatment had not changed. Only as pathogenesis and stimulatory pathways became recognized did surgical and then medical therapy become more focused and more effective.
Diet
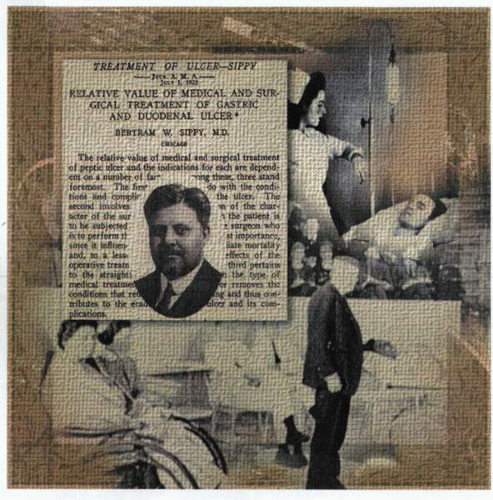
In 1915, Dr. Bertram Sippy advocated hourly feedings of milk, eggs, and purees from 7:00 a.m. to 8:00 p.m. Between these hourly feedings, and every half hour for 2½ hours after the last feeding, Sippy powder (calcium and sodium bicarbonate) was administered. In addition, to relieve dyspepsia, the patient’s stomach was aspirated at regular intervals each night. This regimen provided a challenge both for the patient and for the nursing staff.
An alternative dietary therapy developed by Richard Doll involved the use for up to 3 weeks of continuous milk drips through a nasogastric tube, with or
without alkali. Although this therapeutic strategy seemed to improve the nutritional status of his patients, the obsessive need for dietary management and regulation of alkali intake so interfered with the lifestyle of patients and so often failed to prevent complications from developing that even surgery became a reasonable option.
without alkali. Although this therapeutic strategy seemed to improve the nutritional status of his patients, the obsessive need for dietary management and regulation of alkali intake so interfered with the lifestyle of patients and so often failed to prevent complications from developing that even surgery became a reasonable option.
Surgery
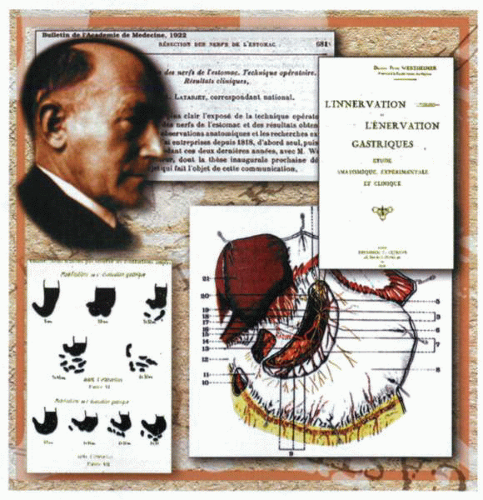
The first dedicated operation was a gastrectomy, but the high morbidity and mortality engendered a degree of caution in both patient and physician alike. Subsequently, vagotomy, which had been initiated in France by Raymond Latarjet and then reactivated in North America by Lester Dragstedt, provided a better alternative for management. Dragstedt’s observations that gastric acid output was decreased by vagotomy were widely cited in favor of this operation. Initial postoperative problems due to decreased gastric emptying were subsequently obviated by the construction of a variety of pyloroplasties to facilitate drainage. Recurrence of peptic ulcer disease and the long-term side effects of the surgery itself show that this therapy option was suboptimal.
Gastroprotection
The evolving trend to use less invasive methodology in the management of peptic ulcer disease resulted in a significant interest in the use of antacids in association with both diet modification and bed rest.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree