Hiatal Hernia Repair
The purpose of hiatal hernia repair is to generate a functional lower esophageal sphincter mechanism that will effectively prevent reflux of gastric contents into the esophagus but will allow swallowing, belching, and vomiting.
Most hiatal hernia repairs are performed laparoscopically (see Chapter 47). Open repair is still necessary when the laparoscopic approach fails or is not feasible. The transabdominal Nissen procedure is presented in this chapter. For this repair, a 360-degree wrap of gastric fundus is placed around the distal esophagus, producing a functional valve. As intragastric pressure increases, the pressure in the wrap increases as well, closing off the distal esophagus. Other surgical techniques for hiatal hernia repair are detailed in the references.
Steps in Procedure
Expose esophageal hiatus (this may require mobilizing the left lobe of the liver)
Incise the peritoneum over the esophagus
Gently isolate the esophagus from surrounding tissues and pass Penrose drain behind it
Divide short gastric vessels to fully mobilize fundus of stomach
Pass dilator transesophageally (or place dilator in operative field—see below)
Pass stomach behind esophagus
Place Hegar dilater next to esophagus (if dilator not passed previously)
Suture stomach to itself over esophagus and dilator
Anchor with one or two sutures that include esophageal wall
Hallmark Anatomic Complications
Injury to esophagus
Injury to vagus nerves
Injury to spleen
Bleeding from short gastric vessels
Entry into either or both pleural cavities
List of Structures
Xiphoid process
Costal margin
Diaphragm
Median arcuate ligament
Esophageal hiatus
Mediastinum
Pericardium
Phrenic nerve
Left and right pleural cavities
Thoracic duct
Inferior vena cava
Aorta
Left inferior phrenic artery (and vein)
Celiac trunk
Left gastric artery
Splenic artery
Short gastric arteries
Left gastroepiploic artery
Superior epigastric artery
Liver
Left lobe
Left triangular ligament
Esophagus
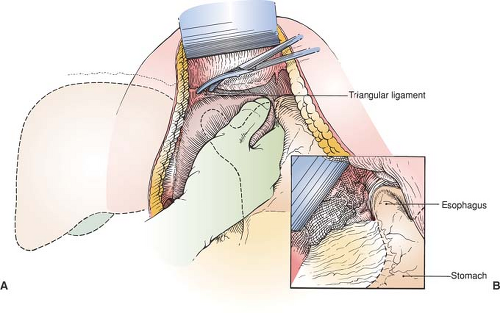
Exposure of the Cardioesophageal Junction (Fig. 46.1)
Technical Points
The right-handed surgeon should stand on the right side of the patient. Make an upper midline laparotomy incision. Extend the incision up and to the left of the xiphoid process for a little additional exposure. Clamp and ligate the small vessels that are frequently encountered in the angle between the xiphoid and costal margin. Do not divide the xiphoid: this adds little to the exposure and may stimulate heterotopic bone formation within the incision. Explore the abdomen and confirm the position of a
nasogastric tube at the cardioesophageal junction. Place a fixed retractor (such as the Omni system) to provide strong cephalad retraction of the left costal margin, placing additional blades to hold the incision open in the midportion. If this type of retractor is not available, a satisfactory alternative is an “upper-hand” type of retractor in the left upper margin of the incision and a Balfour retractor in the middle of the incision. Reverse Trendelenburg position assists as gravity pulls the upper abdominal viscera caudad into the field.
nasogastric tube at the cardioesophageal junction. Place a fixed retractor (such as the Omni system) to provide strong cephalad retraction of the left costal margin, placing additional blades to hold the incision open in the midportion. If this type of retractor is not available, a satisfactory alternative is an “upper-hand” type of retractor in the left upper margin of the incision and a Balfour retractor in the middle of the incision. Reverse Trendelenburg position assists as gravity pulls the upper abdominal viscera caudad into the field.
In most cases, adequate exposure can be obtained by placing a liver blade under the left lobe and retracting it upward. If exposure is not sufficient, mobilize the left lobe of the liver by incising the triangular ligament. Pass your left hand around the inferior edge of the left lobe of the liver, grasp it, and pull down. The triangular ligament will be seen as a thin, tough, membranous structure passing along the posterosuperior aspect of the liver. Divide the small vessel at the free edge between hemoclips. Use electrocautery to divide the triangular ligament. As you progress to the right, an anterior and posterior leaf of the triangular ligament will become apparent, with loose areolar tissue between. At this point, continue the dissection cautiously with Metzenbaum scissors until the left lobe of the liver can be folded down to expose the cardioesophageal junction. Place a moist laparotomy pad and Harrington retractor over the left lobe of the liver to hold it out of the way.
The inferior aspect of the diaphragm and the cardioesophageal junction should now be clearly visible. Confirm the location of the esophagus by palpating the nasogastric tube, which is anterior and a little to the left of the aorta at the esophageal hiatus. Incise the peritoneum overlying the cardioesophageal junction to expose the esophagus. Take care to avoid injury to the vagal nerve trunks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree