Hand-Assisted Laparoscopic Sigmoidectomy
Daniel A. Anaya
Daniel Albo
DEFINITION
A sigmoidectomy is the resection of the sigmoid colon to the level of the rectosigmoid junction. The extent of the lymphadenectomy will be determined by the indication (benign vs. malignant disease).
Focal segmental sigmoid resection for benign disease can be accomplished by dividing the vessels close to the bowel wall, without the need for a high pedicle transection. A complete sigmoidectomy (described in this chapter) includes transection of the inferior mesenteric artery (IMA) at its origin and resection of the proximal superior hemorrhoidal artery (SHA) and sigmoidal branches.
A hand-assisted laparoscopic (HAL) sigmoidectomy approach uses a hand access port to aid with the dissection and resection. This approach increases the use of minimally invasive surgery, reduces conversion rates, and decreases operative times while maintaining all the short-term outcome advantages when compared to conventional laparoscopic surgery.
DIFFERENTIAL DIAGNOSIS
Indications for sigmoidectomy include the following:
Sigmoid colon polyps and cancer
Diverticular disease (i.e., complicated diverticulitis, perforation, fistulae, etc.)
Other indications include sigmoid volvulus, ischemic or infectious colitis, and trauma.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients with sigmoid pathology can be asymptomatic, with abnormalities found during screening colonoscopy.
The most common symptoms are bleeding (occult/anemia or overt), obstruction, and pain.
The initial history should include the following:
Time course of presenting symptoms, including bleeding, constipation, and pain
Presence/absence of rectal incontinence
History of sexual function (erection and ejaculation for males, dyspareunia for females)
Information regarding associated urologic symptoms such as recurrent urinary tract infections, dysuria, pneumaturia and/or fecaluria, which suggest a possible fistula with the urinary tract
Presence of systemic symptoms such as fever and weight loss
Previous surgical history, specifically regarding abdominal and/or pelvic surgery
Personal and/or family history of prior colon cancer/polyps, inflammatory bowel disease, diverticular disease
The physical exam should include the following:
Focused abdominal exam, including notation of abdominal scars
Digital rectal exam, focused on assessment of sphincter function
Rigid proctoscopy, for all patients with sigmoid polyps or cancer reported by endoscopy to be within 20 cm from the anal verge. This will allow for confirmation of the site of the lesion, which oftentimes may not coincide with the endoscopy report. This information may alter the surgical and oncologic approach.
Rigid proctoscopy should not be performed in patients presenting with acute diverticulitis or perforation to avoid worsening of a microperforation by air insufflation.
IMAGING AND OTHER DIAGNOSTIC STUDIES
A complete colonoscopy should be performed to rule out synchronous disease.
For cancer and/or polyps, a tattoo must be placed just distal to the lesion at three different points within the circumference to allow for intraoperative localization of the target.
A computed tomography (CT) of the abdomen and pelvis is obtained to rule out adjacent organ involvement, to evaluate for extraluminal complications (e.g., abscess, fistula), and to rule out metastatic disease in patients with cancer. A CT of the chest completes the metastatic workup.
A carcinoembryonic antigen (CEA) level is obtained in all cancer cases.
SURGICAL MANAGEMENT
Preoperative Planning
An informed consent, including discussion of the need for a possible ostomy, is obtained.
We do not routinely ask patients to complete a formal bowel preparation. Fleet enemas are prescribed to facilitate the performance of the anastomosis.
All patients should receive preoperative prophylactic antibiotics, following published guidelines. We administer 1 to 2 g of ertapenem within 1 hour of surgical incision.
Pharmacologic deep vein thrombosis (DVT) prophylaxis should be given to patients perioperatively, based on current recommendations and guidelines.
Patient Positioning and Operating Room Setup
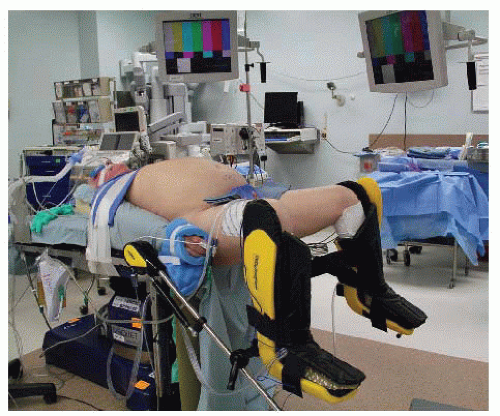
Proper patient position and operating room (OR) setup is critical for successful performance of minimally invasive surgery (FIG 1).
The patient is placed in a modified lithotomy position using Yellofin stirrups with the heels firmly planted in the stirrups.
Pressure-bearing areas in the calf and lateral legs are padded to prevent DVT and lateral peroneal nerve injury.
The patient’s toes, knee, and contralateral shoulder are aligned.
The thighs are placed parallel to the ground to prevent conflict with the surgeon’s arms.
The patient’s buttocks are placed at the edge of the table to allow for smoother introduction of the end-to-end anastomosis (EEA) stapler at time of reconstruction.
Both arms are tucked at the sides, with padding added to protect against nerve injuries.
The patient is taped to the table across the chest over towels to avoid slipping.
All laparoscopic elements (CO2 line, camera, light cord) exit through the right upper side. All energy device cords exit through the upper left side. This allows for a clutter-free working space for the operative team.
Team Positioning and Draping
The patient is prepped with chlorhexidine and draped to facilitate easy access to the perineum.
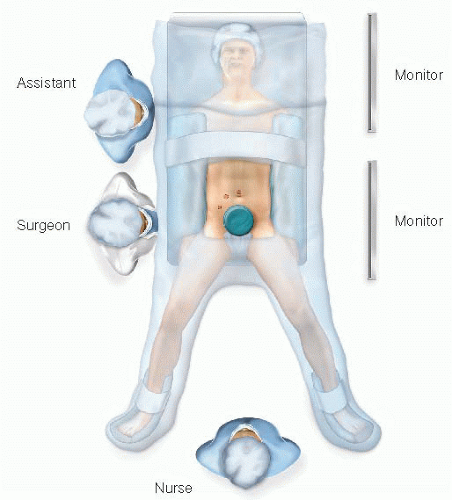
The surgeon stands at the patient’s right lower side, with the assistant to his or her left side and the scrub nurse to his or her right side (FIG 2).
Two monitors are placed in front of the team at eye level on the patient’s left side.
TECHNIQUES
PORT PLACEMENT
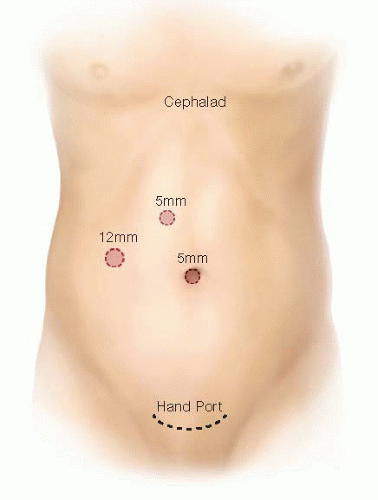
Insert the GelPort through a 5- to 6-cm Pfannenstiel incision. This incision will be also used for specimen extraction. It results in better cosmesis, lowers the incidence of wound infections and hernias, and allows for more working space between the hand and the instruments.
Ports: Insert a 5-mm working port in the right upper quadrant (RUQ), a 12-mm working port in the right lower quadrant, and a 5-mm camera port above the umbilicus. These three ports are triangulated, with the camera port at the apex of the triangle. This setup avoids conflict between instruments and camera and prevents disorientation (avoids “working on a mirror”) (FIG 3).
OPERATIVE STEPS
Our HAL sigmoidectomy operation is highly standardized and consists of nine steps:
Transection of the inferior mesenteric vein (IMV)
Transection of the IMA
Medial to lateral dissection of the descending mesocolon
Sigmoid colon mobilization off the pelvic inlet
Descending colon mobilization
Mobilization of the splenic flexure
Intracorporeal distal transection
Extracorporeal proximal transection
Intracorporeal anastomosis
Step 1. Transection of the Inferior Mesenteric Vein
This is the critical “point of entry” in this operation. We favor it over starting at the IMA level due to the IMV’s constancy in location, the ease of its visualization by the ligament of Treitz, and the absence of structures that can be harmed around it (no iliac vessels or left ureter nearby). This will be the only time during the operation when a virgin tissue plane is entered. Every step will set up the following ones, opening the tissue planes sequentially.
The patient is placed on a steep Trendelenburg position with the left side up. Using the right hand, move the small bowel into the RUQ and the transverse colon and omentum into the upper abdomen. If necessary, place a laparotomy pad to hold the bowel out of the field of view, especially in obese patients. This pad can also be used to dry up the field and to clean the scope tip intracorporeally. Make sure the circulating nurse notes the laparotomy pad in the abdomen on the white board.
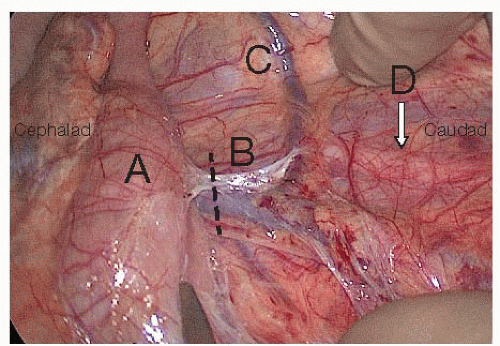
Identify the critical anatomy: IMV, ligament of Treitz, and left colic artery (FIG 4).
If there are attachments between the duodenum/root of mesentery and mesocolon, transect them with laparoscopic scissors. This will allow for adequate exposure of midline structures.
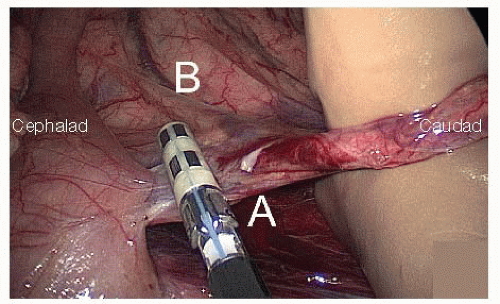
FIG 5 • Step 1: The surgeon holds the IMV (A) anteriorly with his or her right hand and transects it cephalad of the left colic artery (B) with a 5-mm energy device.
Pick up the IMV with the right hand. Incise the peritoneum under the IMV and dissect in front of Gerota’s fascia with endoscopic scissors, starting at the level of the ligament of Treitz. Proceed with the dissection caudally towards the IMA. The assistant provides upward countertraction with a grasper.
Transect the IMV (FIG 5) cephalad of left colic artery, which moves away from the IMV and toward the splenic flexure of the colon, with the 5-mm energy device, thus preserving intact the left-sided marginal arterial arcade, and preserving the blood supply to the anastomosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree