Hand-Assisted Laparoscopic Abdominoperineal Resection
Daniel Albo
DEFINITION
An abdominoperineal resection, or APR, involves removal of the anus, the rectum, and part or all of the sigmoid colon along with the associated regional lymph nodes, through incisions made in the abdomen and perineum. The end of the remaining colon is brought out as a colostomy.
Hand-assisted laparoscopic surgery (HALS) is a minimally invasive surgical approach that uses conventional laparoscopic-assisted (LA) surgery techniques with the addition of a hand-assist device (placed in the projected specimen extraction site) that allows for the introduction of a hand into the surgical field. HALS in colorectal surgery retains all of the same advantages of conventional LA surgery over open surgery, including less pain, faster recovery, lower incidence of wound complications, and reduction of cardiopulmonary complications, especially in the obese and in the elderly.
Advantages of HALS over conventional LA colorectal surgery include the following:
Reintroduces tactile feedback into the field
Shorter learning curves; easier to teach
Shorter operative times and lower conversion to open rates
Higher usage rates of minimally invasive surgery
DIFFERENTIAL DIAGNOSIS
Indications for HALS APR
Rectal cancer: when unable to obtain a negative distal margin and/or in patients with poor sphincter function or severe comorbidities
Anal cancer: after failure of chemotherapy/radiation therapy or in the palliative setting
Inflammatory bowel disease (i.e., Crohn’s with severe perianal disease)
PATIENT HISTORY AND PHYSICAL FINDINGS
Most patients with rectal tumors generally present after an incidental finding during screening colonoscopy or with occult bleeding and anemia.
A thorough history and physical examination should include the following:
Presence of rectal pain and/or tenesmus
Presence of obstructive symptoms
Description of anorectal function, with any fecal incontinence or leakage documented preoperatively
Documentation of urinary and erectile function/dysfunction
A detailed personal and family history of colorectal cancer, polyps, and/or other malignancies
Physical examination should include the following:
Routine abdominal examination, noting any previous incisions
Digital rectal examination with assessment of sphincter function
Bilateral inguinal nodal examination
Rigid proctoscopy is arguably the most critical portion of the physical examination and is the key to proper patient selection of patients for an APR.
Proctoscopy should be standardized and documented at minimum.
The distal and proximal extent of the lesion measured from the anal verge
Exact position of the lesion and extent of the rectal circumference involved
Presence or absence of fixation to perirectal structures
IMAGING AND OTHER DIAGNOSTIC STUDIES
A colonoscopy with documentation of all polyps should be performed. Suspicious lesions should be tattooed to facilitate localization during surgery.
Staging with endorectal ultrasound or rectal magnetic resonance imaging (MRI) should be performed to determine the need for neoadjuvant therapy and to plan operative strategy. A computed tomography (CT) of the chest, abdomen, and pelvis evaluates for potential metastases.
A preoperative carcinoembryonic antigen level should be obtained.
SURGICAL MANAGEMENT
Preoperative Preparation
Patients undergo stoma marking by an enterostomal therapist.
Clinical trials have shown no need for mechanical bowel preparation.
We use two fleet enemas to evacuate the rectal vault prior to surgery.
Intravenous cefoxitin is administered within 1 hour of skin incision.
Use hair clippers if needed and chlorhexidine gluconate skin preparation.
Preoperative time-out and briefing is performed.
Ultrasound-guided, bilateral transversus abdominis plane (TAP) block reduces the need for postoperative narcotics.
Equipment and Instrumentation
5-mm camera with high-resolution monitors
5-mm and 12-mm clear ports with balloon tips. They hold ports in the abdomen and minimize their intraabdominal profile during surgery.
Laparoscopic endoscopic scissors and a blunt tip 5-mm energy device
60-mm linear reticulating laparoscopic staplers with vascular and tan loads
We use the GelPort hand-assist device due to its versatility and ease of use. This device allows for the introduction/removal of the hand without losing pneumoperitoneum and
allows for insertion of multiple ports through the hand-assist device. It also allows for the introduction of laparotomy pads into the field, which are very useful to retract bowel/omentum in obese patients.
Patient Positioning and Surgical Team Setup
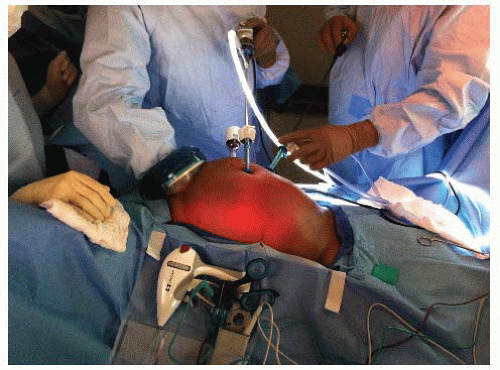
Place the patient on a modified lithotomy position, with the arms tucked and padded (to avoid nerve/tendon injuries). The patient is taped over a towel across the chest without compromising chest expansion (FIG 1).
Place the legs on Allen stirrup with the heels firmly planted on the stirrups to avoid pressure on the calves and the lateral peroneal nerves.
Keep the thighs parallel to the ground to avoid conflict between the thighs and the surgeon’s arms/instruments.
The coccyx should be readily palpable off the edge of the table. This will be critical for the perineal step of the operation.
The surgeon starts at the patient’s right lower side with the assistant to his or her left side.
Align the surgeon, the ports, the targets, and the monitors in straight lines. Place monitors in front of the surgeon and at eye level to prevent lower neck stress injuries.
Avoid unnecessary restrictions to potential team movement around the table. All energy device cables exit by the patient’s upper left side. All laparoscopic (gas, light cord, and camera) elements exit by the patient’s upper right side.
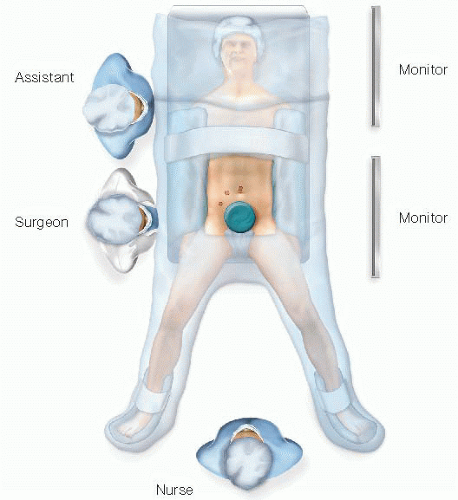 FIG 1 • Team, patient, and monitor setup. The patient is on a modified lithotomy position. The team, ports, targets, and monitors are aligned. |
TECHNIQUES
PORT PLACEMENT AND OPERATIVE FIELD SETUP
Insert the GelPort through a 5- to 6-cm Pfannenstiel incision. This incision will be also used for specimen extraction. It provides a better cosmetic result and lowers the incidence of wound infections and hernias. It also allows for more working space between the hand and the instruments. (FIGS 1 and 2).
Ports: Insert a 5-mm working port in the right upper quadrant, a 12-mm working port in the right lower quadrant, and a 5-mm camera port above the umbilicus. These three ports are triangulated, with the camera port at the apex of the triangle. This setup avoids conflict between the instruments and the camera and prevents disorientation (avoids “working on a mirror”).
A 5-mm accessory working port may be inserted at the planned colostomy site in the left lower quadrant (LLQ). This port allows the surgeon to operate from the left side of the table (useful for the right-sided pelvic dissection, especially in males). It can also be valuable for the mobilization of the splenic flexure.
OPERATIVE STEPS
Our HALS APR operation is highly standardized and consists of eight steps:
Transection of the inferior mesenteric vein (IMV)
Transection of the inferior mesenteric artery (IMA)
Medial to lateral dissection of the descending mesocolon
Sigmoid colon mobilization off the pelvic inlet
Descending colon mobilization
Pelvic dissection
Transection of the levator ani muscles
Creation of colostomy and closure of abdominal wounds
Step 1. Transection of the Inferior Mesenteric Vein
This is the critical “point of entry” in this operation. We favor it over starting dissection at the IMA level due to the IMV’s constancy in location, the ease of its visualization by the ligament of Treitz, and the absence of structures that can be harmed around it (no iliac vessels or left ureter nearby). This will be the only time during the operation when a virgin tissue plane is entered. Every step will set up the following ones, opening the tissue planes sequentially.
The patient is placed on a steep Trendelenburg position with the left side up. Using the right hand, move the small bowel into the right upper quadrant and the transverse colon and omentum into the upper abdomen. If necessary, place a laparotomy pad to hold the bowel out of the field of view, especially in obese patients. This pad can also be used to dry up the field and to clean the scope tip intracorporeally. Make sure that the circulating nurse notes the laparotomy pad in the abdomen on the white board.
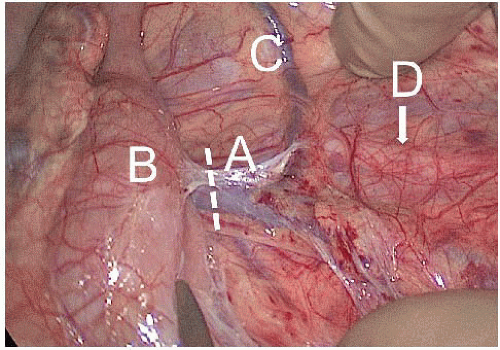
Identify the critical anatomy: IMV, ligament of Treitz, and left colic artery (FIG 3).
If there are attachments between the duodenum/root of mesentery and mesocolon, transect them with laparoscopic scissors. This will allow for adequate exposure of midline structures.
Pick up the IMV with the right hand. Dissect under the IMV and in front of Gerota’s fascia with endoscopic scissors, starting at the level of the ligament of Treitz and proceeding with the dissection caudally toward the IMA. The assistant provides upward countertraction with a grasper.
Transect the IMV cephalad of left colic artery (which moves away from the IMV and toward the splenic flexure of the colon) with the 5-mm energy device, thus preserving intact the left-sided marginal arterial arcade and maintaining the blood supply to the descending colon segment (FIG 4).
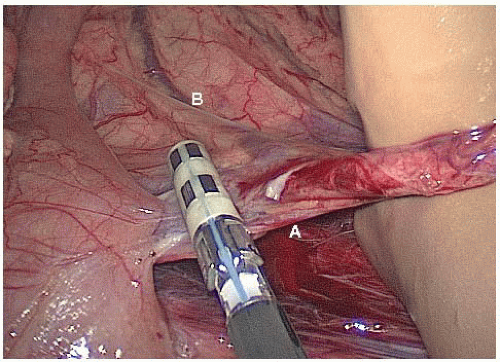 FIG 4 • Step 1: Transection of the IMV (A) cephalad of the left colic artery (B).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|