Graft vs. Host Disease
Julie E. Jackson, MD
Chandra N. Smart, MD
Key Facts
Terminology
Multisystem disease affecting skin and gastrointestinal tract occurring in immunosuppressed transplant recipients
Occurs as a result of immunocompetent donor T-lymphocytes responding to incompatible foreign host major histocompatibility complex (MHC) antigens
Clinical Issues
Most commonly occurs in allogenic bone marrow transplants
Microscopic Pathology
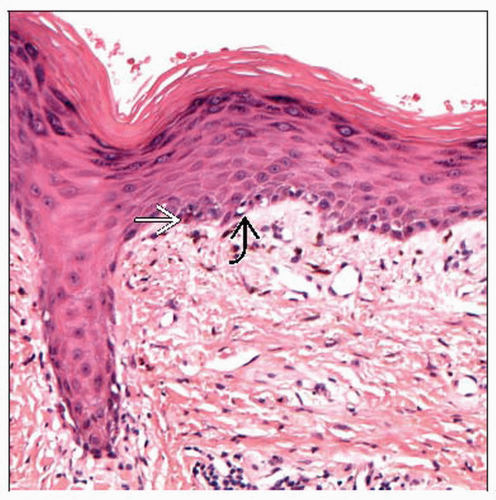
Acute GVHD
Focal or diffuse interface dermatitis with scattered apoptotic keratinocytes closely associated with neighboring lymphocytes (satellite cell necrosis)
Chronic lichenoid GVHD
Parakeratosis, hypergranulosis, and irregular acanthosis with dense dermal lichenoid infiltrate leading to vacuolar interface change with cytoid body formation
Chronic sclerodermoid GVHD
Epidermal atrophy with flattening of rete ridge pattern and marked dermal fibrosis leading to loss of adnexal structures
In either chronic form, other characteristic features of GVHD (including vacuolar interface change, satellite cell necrosis, and perivascular infiltrate) are variably present
TERMINOLOGY
Abbreviations
Graft vs. host disease (GVHD)
Definitions
Multisystem disease affecting skin and gastrointestinal tract, occurring in immunosuppressed transplant recipients
Occurs as a result of immunocompetent donor T lymphocytes responding to incompatible foreign host major histocompatibility complex (MHC) antigens
Acute GVHD
Classically occurs within 100 days of transplant with peak incidence around day 30
Chronic GVHD
Typically occurs within 3-5 months after grafting and primarily consists of either lichen planus-like eruption or sclerodermoid form
ETIOLOGY/PATHOGENESIS
Proposed Immunologic Mechanisms
Donor T-lymphocytes activate and proliferate in setting of immunocompromised host because the host cannot reject the transplanted cells
Pretransplant tissue damage, through radiation or chemotherapy, is thought to increase recognition of host’s antigens by donor’s T-lymphocytes
Donor T-lymphocytes cause host cell death through cytotoxic T-cell effects mediated by perforin, granzyme, and apoptosis through Fas/Fas ligand pathway
Occurrence related to HLA mismatch but minority of cases develop due to mismatch of minor histocompatibility antigens
CLINICAL ISSUES
Presentation
Most commonly occurs in allogenic bone marrow transplants, but also reported in
Solid organ transplantation, severely immunosuppressed patients following transfusion of non-irradiated blood products, transplacentally to immunodeficient fetus, and rarely in autologous transplants
Acute GVHD
Initially, a morbilliform rash characterized by erythematous macules & papules with possible mucosal involvement
Begins with punctate lesions around adnexal structures involving face, trunk, palms, & soles
Can also present as acral erythema, an eczema-like eruption, ichthyosis, or, in severe cases, erythroderma with diffuse desquamation mimicking toxic epidermal necrolysis
Other clinical features include cholestatic hepatitis with increased bilirubin and high-volume diarrhea
Chronic GVHD
Lichenoid chronic GVHD
May present with malar rash and lichen planus-like eruption characterized by brownish to purple flat-topped papules, occurring initially on distal extremities before becoming generalized
With chronicity, skin can become poikilodermatous with atrophy, telangiectasia, and dyspigmentation
Sclerodermoid chronic GVHD
Morphea-like lesions may occur as atrophic shiny plaques with overlying cigarette paper atrophy of skin located in areas of pressure
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree