Glycogen Storage Disease
Grace E. Kim, MD
Key Facts
Etiology/Pathogenesis
Inborn error of carbohydrate metabolism caused by gene mutations in proteins involved in glycogen synthesis, degradation, or regulation
Results in different enzymatic defects in liver that are classified as GSD types 0, I, II, III, IV, VI, and IX
80% of hepatic GSD is types I, III, and IX
Clinical Issues
Most patients present with hepatomegaly and hypoglycemia
Increased incidence of hepatic adenoma and hepatocellular carcinoma in GSD I and also GSD III
Liver transplantation corrects primary hepatic enzyme defect and is used primarily for GSD IV
Microscopic Pathology
Assess liver for mosaic pattern of hepatocytes, glycogenated nuclei, fatty change, and fibrosis
GSD 0 has decreased glycogen
GSD IV has characteristic cytoplasmic inclusions
Cirrhosis occurs frequently in GSD IV and can occur in III and IX
Ancillary Tests
Lysosomal-bound glycogen for GSD II
Fibrillar glycogen for GSD IV
Top Differential Diagnoses
Glycogen hepatopathy
Other entities with ground-glass cytoplasm
TERMINOLOGY
Abbreviations
Glycogen storage disease (GSD)
Synonyms
Glycogenoses
ETIOLOGY/PATHOGENESIS
Inborn Error of Carbohydrate Metabolism
Gene mutation in proteins involved in glycogen synthesis, degradation, or regulation
Hepatic enzyme deficiency
GSD types 0, I, II, III, IV, VI, and IX
80% of hepatic GSD is types I, III, and IX
Abnormal concentration or structure of glycogen
GSD 0 results in decreased hepatic glycogen
Remaining types of GSD display increased hepatic glycogen
Inherited as autosomal recessive trait
Exception is GSD IX (X-linked disorder)
CLINICAL ISSUES
Presentation
Hepatomegaly
Occurs in GSD I, III, IV, VI, and IX
Rarely in GSD II
Not in GSD 0
Hypoglycemia
Occurs in GSD 0, I, and III
Mild in VI and IX
Rarely in GSD IV
Not in GSD II
Laboratory Tests
Confirmation of diagnosis
Enzymatic assay on liver
GSD 0, I, II, III, VI, and IX
DNA mutation analysis
Treatment
Options, risks, complications
Increased incidence of hepatocellular neoplasia
Hepatic adenoma is frequent in GSD I and can occur in GSD III
Hepatocellular carcinoma occurs in GSD I and is reported in GSD III
GSD Ib has been associated with Crohn-like disease
Granulomatous colitis
Responds to inflammatory bowel disease treatment regimen
Dietary intervention
Prevent hypoglycemia, particularly for GSD 0 and I, less stringent in GSD III
Surgical approaches
Liver transplantation corrects primary hepatic enzyme defect
Has been performed for GSD I, III, and IV
Best treatment option for GSD IV
Prognosis
Variable based on type of GSD
GSD II (infantile form) usually results in death in 1st year of life
GSD IV (classic hepatic form) has rapid disease progression with liver failure from 3-5 years of age
MICROSCOPIC PATHOLOGY
Histologic Features
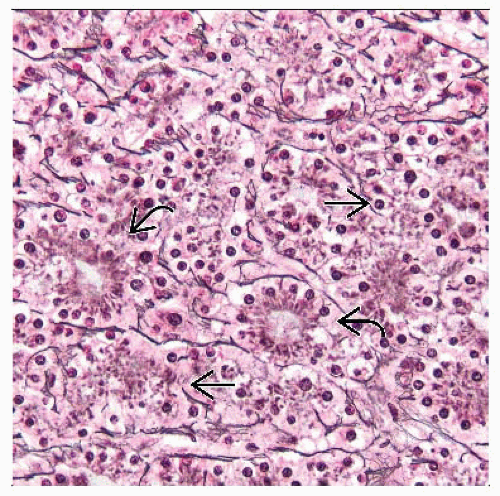
Histologic features are not generally diagnostic of GSD
Exception is characteristic cytoplasmic inclusion in GSD IV
Weakly basophilic to colorless inclusion, retracts from surrounding cytoplasm
PAS positive and partially digested on PAS-D
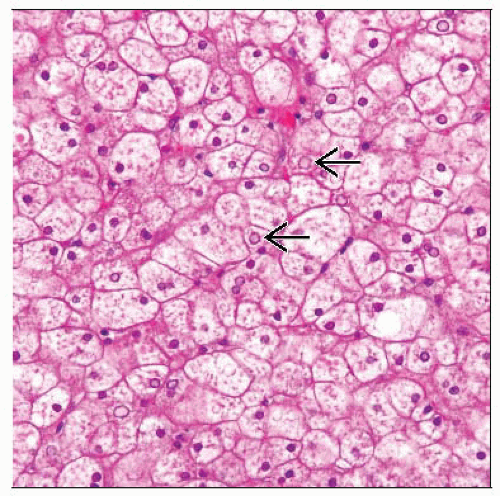
Mosaic architecture
In GSD I, III, VI, and IX
Attributed to enlarged, pale-staining, swollen hepatocytes
Compression of sinusoid by expanded hepatocytes
Excess glycogen is PAS positive, PAS-D negative
Glycogen may wash out with formalin processing
Glycogen can be retained with alcohol fixation
Fibrosis
Initially in periportal region
GSD III, IV, VI, IX; may occur in GSD I
Frequently progresses to cirrhosis in GSD IV
Cirrhosis can occur in III and IX
Features of hepatocytes
Glycogenated nuclei
In GSD I (prominent) and III (less)
Thickened cytoplasmic membrane
Resulting from organelles at periphery of cytoplasm
Cytoplasmic lipid in all GSD
More pronounced in GSD I
Ultrastructural Features
GSD 0
Nonspecific with sparse glycogen
GSD I
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree