Glomangiopericytoma (Sinonasal-type Hemangiopericytoma)
Lester D. R. Thompson, MD
Key Facts
Terminology
Soft tissue tumor showing perivascular myoid differentiation
Clinical Issues
Nasal cavity is usually affected in isolation
Present with nasal obstruction and epistaxis
Excellent long-term outcome with surgery alone, although recurrences develop
Macroscopic Features
Tends to be polypoid mass about 3 cm
Microscopic Pathology
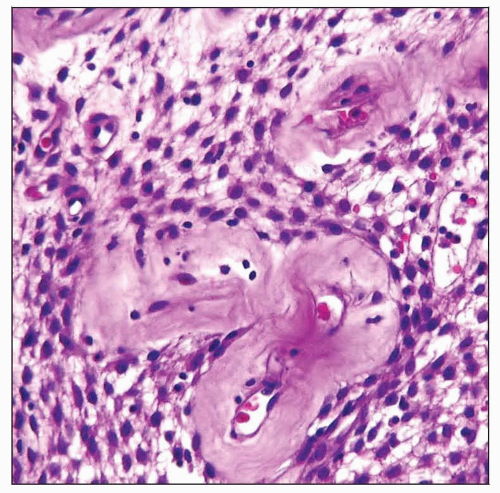
Peritheliomatous (perivascular) hyalinization is characteristic
Cellular, diffuse, syncytial arrangement
Surface epithelium usually intact (respiratory type or metaplastic squamous mucosa)
Many patterns of growth, often within same tumor
Ramifying, branching pattern of vessels
Mixture of inflammatory cells in background
Eosinophils, mast cells, and lymphocytes, although first two predominate
Extravasated erythrocytes
Ancillary Tests
Shows myoid phenotype (actins positive)
Lacks vascular markers (CD34, CD31, FVIIIRAg)
Top Differential Diagnoses
Lobular capillary hemangioma
Solitary fibrous tumor
Nasopharyngeal angiofibroma
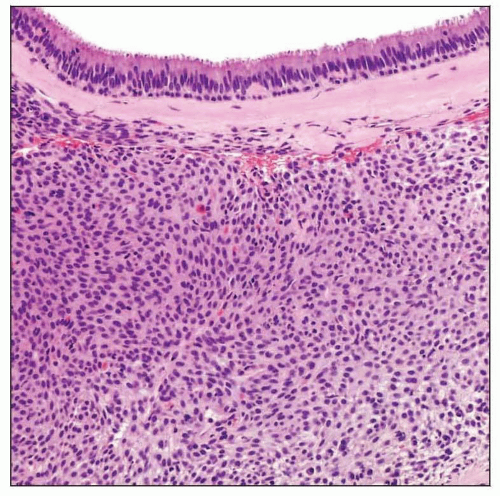 Hematoxylin & eosin shows an intact, uninvolved respiratory epithelium subtended by a thick band of fibrosis. Below this is a patternless, bland, cellular proliferation. |
TERMINOLOGY
Abbreviations
Sinonasal-type hemangiopericytoma (SNTHPC)
Synonyms
Sinonasal hemangiopericytoma-like tumor
Glomus tumor
Hemangiopericytoma
Solitary fibrous tumor (inaccurate in sinonasal site)
Intranasal myopericytoma
Definitions
Soft tissue tumor showing perivascular myoid differentiation defined by glomus (myoid) and hemangiopericytoma (pericyte) features within same lesion
ETIOLOGY/PATHOGENESIS
Myopericyte
May arise from plentiful pericytes associated with vessels of nasal cavity
CLINICAL ISSUES
Epidemiology
Incidence
Rare, comprising < 0.5% of sinonasal primary neoplasms
Age
Broad range at presentation (5-90 years old)
Mean: 7th decade
Age at presentation does not affect prognosis
Gender
Female > Male (1.2:1)
No difference in outcome based on gender
Site
Nasal cavity is usually affected in isolation
Turbinate and septum are occasionally affected in isolation
Maxillary and ethmoid sinuses may also be affected in conjunction with nasal cavity
Bilateral tumors are uncommon (approximately 5%)
Presentation
Nasal obstruction
Epistaxis
Mass, polyps
Difficulty breathing
Sinusitis
Headache, congestion, pain
Discharge
Changes in smell
Symptoms usually present for < 1 year
Rare association with osteomalacia
Treatment
Options, risks, complications
Surgery is treatment of choice, although radiation has been used in nonsurgical candidates
Chemotherapy is not used
Surgical approaches
Polypectomy or wide surgical excision
Complete surgical extirpation decreases risk of recurrence (residual or recrudescence)
Prognosis
Excellent long-term survival (5-year survival ˜ 90%)
Recurrences may develop (˜ 18%)
Multiple recurrences may be seen
Recurrences are associated with
Long duration of symptoms
Bone invasion
Severe nuclear pleomorphism
Long-term clinical follow-up advocated as recurrences may develop late
IMAGE FINDINGS
CT Findings
Nasal cavity opacification by polypoid mass accompanied by bone erosion or sclerosis
Destructive mass of nasal cavity and paranasal sinuses
No cribriform plate involvement
Angiograms show tumor blush
Nonspecific sinusitis frequently concurrent
MACROSCOPIC FEATURES
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree