KEY POINTS
The physiology of the gallbladder and sphincter of Oddi is regulated by a complex interplay of hormones and neuronal inputs designed to coordinate bile release with food consumption. Dysfunctions related to this activity are linked to the development of gallbladder pathologies described in this chapter.
In Western countries, the most common type of gallstones are cholesterol stones. The pathogenesis of these stones relates to supersaturation of bile with cholesterol and subsequent precipitation.
Laparoscopic cholecystectomy has been demonstrated to be a safe and effective alternative to open cholecystectomy and has become the treatment of choice for symptomatic gallstones. Knowledge of the various anatomic anomalies of the cystic duct and artery is helpful in guiding the dissection of these structures as well as avoiding injury to the common bile duct during cholecystectomy.
Common bile duct injuries, although uncommon, can be devastating to patients. Proper exposure of Calot’s triangle and careful identification of the anatomic structures are keys to avoiding these injuries. Once a bile duct injury is diagnosed, the best outcomes are seen at large referral centers with experienced biliary surgeons.
The main risk factor for gallbladder disease in Western countries is cholelithiasis. The main complications include cholecystitis, choledocholithiasis, cholangitis, and biliary pancreatitis. In addition, cholelithiasis plays the role as the major risk factor for the development of gallbladder cancer.
Carcinoma of the gallbladder and bile duct generally have a poor prognosis because patients usually present late in the disease process and have poor response to chemotherapy and radiation therapy. Surgery offers the best chance for survival and has good long-term survival in patients with early-stage disease.
ANATOMY
The gallbladder is a pear-shaped sac, about 7 to 10 cm long, with an average capacity of 30 to 50 mL. When obstructed, the gallbladder can distend markedly and contain up to 300 mL.1 The gallbladder is located in a fossa on the inferior surface of the liver. A line from this fossa to the inferior vena cava divides the liver into right and left liver lobes. The gallbladder is divided into four anatomic areas: the fundus, the corpus (body), the infundibulum, and the neck. The fundus is the rounded, blind end that normally extends 1 to 2 cm beyond the liver’s margin. It contains most of the smooth muscles of the organ, in contrast to the body, which is the main storage area and contains most of the elastic tissue. The body extends from the fundus and tapers into the neck, a funnel-shaped area that connects with the cystic duct. The neck usually follows a gentle curve, the convexity of which may be enlarged to form the infundibulum or Hartmann’s pouch. The neck lies in the deepest part of the gallbladder fossa and extends into the free portion of the hepatoduodenal ligament (Fig. 32-1).
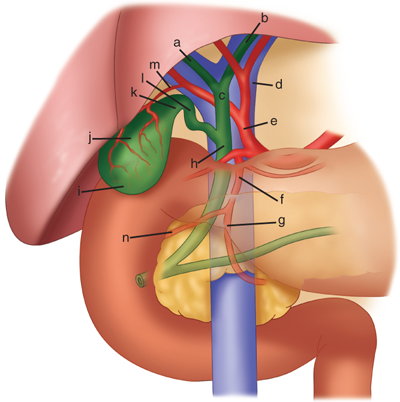
Figure 32-1.
Anterior aspect of the biliary anatomy. a = right hepatic duct; b = left hepatic duct; c = common hepatic duct; d = portal vein; e = hepatic artery; f = gastroduodenal artery; g = left gastric artery; h = common bile duct; i = fundus of the gallbladder; j = body of gallbladder; k = infundibulum; l = cystic duct; m = cystic artery; n = superior pancreaticoduodenal artery. Note the situation of the hepatic bile duct confluence anterior to the right branch of the portal vein, and the posterior course of the right hepatic artery behind the common hepatic duct.
The same peritoneal lining that covers the liver covers the fundus and the inferior surface of the gallbladder. Occasionally, the gallbladder has a complete peritoneal covering and is suspended in a mesentery off the inferior surface of the liver, and rarely, it is embedded deep inside the liver parenchyma (an intrahepatic gallbladder).
The gallbladder is lined by a single, highly folded, tall columnar epithelium that contains cholesterol and fat globules. The mucus secreted into the gallbladder originates in the tubuloalveolar glands found in the mucosa lining the infundibulum and neck of the gallbladder, but are absent from the body and fundus. The epithelial lining of the gallbladder is supported by a lamina propria. The muscle layer has circular longitudinal and oblique fibers, but without well-developed layers. The perimuscular subserosa contains connective tissue, nerves, vessels, lymphatics, and adipocytes. It is covered by the serosa except where the gallbladder is embedded in the liver. The gallbladder differs histologically from the rest of the gastrointestinal (GI) tract in that it lacks a muscularis mucosa and submucosa.
The cystic artery that supplies the gallbladder is usually a branch of the right hepatic artery (>90% of the time). The course of the cystic artery may vary, but it nearly always is found within the hepatocystic triangle, the area bound by the cystic duct, common hepatic duct, and the liver margin (triangle of Calot). When the cystic artery reaches the neck of the gallbladder, it divides into anterior and posterior divisions. Venous return is carried either through small veins that enter directly into the liver or, rarely, to a large cystic vein that carries blood back to the portal vein. Gallbladder lymphatics drain into nodes at the neck of the gallbladder. Frequently, a visible lymph node overlies the insertion of the cystic artery into the gallbladder wall. The nerves of the gallbladder arise from the vagus and from sympathetic branches that pass through the celiac plexus. The preganglionic sympathetic level is T8 and T9. Impulses from the liver, gallbladder, and the bile ducts pass by means of sympathetic afferent fibers through the splanchnic nerves and mediate the pain of biliary colic. The hepatic branch of the vagus nerve supplies cholinergic fibers to the gallbladder, bile ducts, and liver. The vagal branches also have peptide-containing nerves containing agents such as substance P, somatostatin, enkephalins, and vasoactive intestinal polypeptide.2
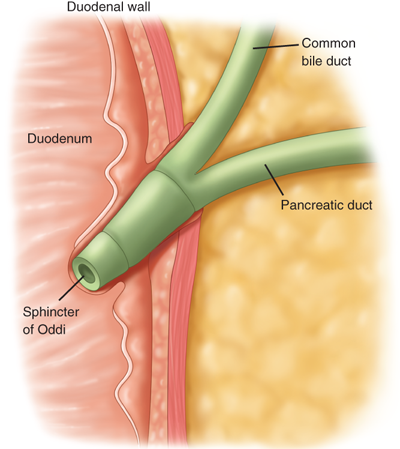
The extrahepatic bile ducts consist of the right and left hepatic ducts, the common hepatic duct, the cystic duct, and the common bile duct or choledochus. The common bile duct enters the second portion of the duodenum through a muscular structure, the sphincter of Oddi.3
The left hepatic duct is longer than the right and has a greater propensity for dilatation as a consequence of distal obstruction. The two ducts join to form a common hepatic duct, close to their emergence from the liver. The common hepatic duct is 1 to 4 cm in length and has a diameter of approximately 4 mm. It lies in front of the portal vein and to the right of the hepatic artery. The common hepatic duct is joined at an acute angle by the cystic duct to form the common bile duct.
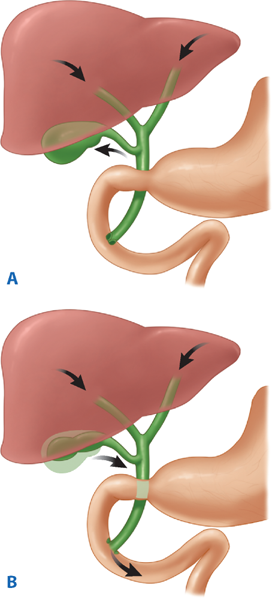
The length of the cystic duct is quite variable. It may be short or absent and have a high union with the hepatic duct, or long and run parallel, behind, or spiral to the main hepatic duct before joining it, sometimes as far as at the duodenum. Variations of the cystic duct and its point of union with the common hepatic duct are surgically important (Fig. 32-2). The segment of the cystic duct adjacent to the gallbladder neck bears a variable number of mucosal folds called the spiral valves of Heister. They do not have any valvular function but may make cannulation of the cystic duct difficult.
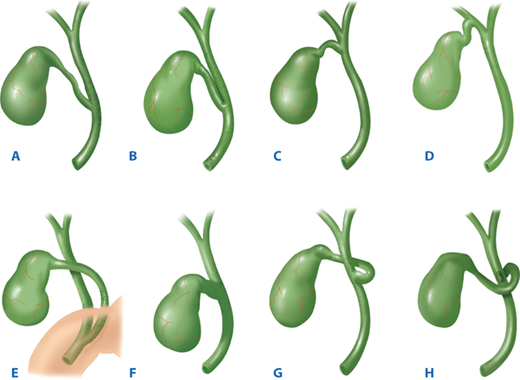
Figure 32-2.
Variations of the cystic duct anatomy. A. Low junction between the cystic duct and common hepatic duct. B. Cystic duct adherent to the common hepatic duct. C. High junction between the cystic and the common hepatic duct. D. Cystic duct drains into right hepatic duct. E. Long cystic duct that joins common hepatic duct behind the duodenum. F. Absence of cystic duct. G. Cystic duct crosses posterior to common hepatic duct and joins it anteriorly. H. Cystic duct courses anterior to common hepatic duct and joins it posteriorly.
The common bile duct is about 7 to 11 cm in length and 5 to 10 mm in diameter. The upper third (supraduodenal portion) passes downward in the free edge of the hepatoduodenal ligament, to the right of the hepatic artery and anterior to the portal vein. The middle third (retroduodenal portion) of the common bile duct curves behind the first portion of the duodenum and diverges laterally from the portal vein and the hepatic arteries. The lower third (pancreatic portion) curves behind the head of the pancreas in a groove, or traverses through it and enters the second part of the duodenum. There, the pancreatic duct frequently joins it. The common bile duct runs obliquely downward within the wall of the duodenum for 1 to 2 cm before opening on a papilla of mucous membrane (ampulla of Vater), about 10 cm distal to the pylorus. The union of the common bile duct and the main pancreatic duct follows one of three configurations. In about 70% of people, these ducts unite outside the duodenal wall and traverse the duodenal wall as a single duct. In about 20%, they join within the duodenal wall and have a short or no common duct, but open through the same opening into the duodenum. In about 10%, they exit via separate openings into the duodenum. The sphincter of Oddi, a thick coat of circular smooth muscle, surrounds the common bile duct at the ampulla of Vater (Fig. 32-3). It controls the flow of bile, and in some cases pancreatic juice, into the duodenum.
The extrahepatic bile ducts are lined by a columnar mucosa with numerous mucous glands in the common bile duct. A fibroareolar tissue containing scant smooth muscle cells surrounds the mucosa. A distinct muscle layer is not present in the human common bile duct. The arterial supply to the bile ducts is derived from the gastroduodenal and the right hepatic arteries, with major trunks running along the medial and lateral walls of the common duct (sometimes referred to as 3 o’clock and 9 o’clock). These arteries anastomose freely within the duct walls. The density of nerve fibers and ganglia increases near the sphincter of Oddi, but the nerve supply to the common bile duct and the sphincter of Oddi is the same as for the gallbladder.1,2
The classic description of the extrahepatic biliary tree and its arteries applies only in about one third of patients.4 The gallbladder may have abnormal positions, be intrahepatic, be rudimentary, have anomalous forms, or be duplicated. Isolated congenital absence of the gallbladder is very rare, with a reported incidence of 0.03%. Before the diagnosis is made, the presence of an intrahepatic bladder or anomalous position must be ruled out. Duplication of the gallbladder with two separate cavities and two separate cystic ducts has an incidence of about one in every 4000 persons. This occurs in two major varieties: the more common form in which each gallbladder has its own cystic duct that empties independently into the same or different parts of the extrahepatic biliary tree, and as two cystic ducts that merge before they enter the common bile duct. Duplication is only clinically important when some pathologic processes affect one or both organs. A left-sided gallbladder with a cystic duct emptying into the left hepatic duct or the common bile duct and a retrodisplacement of the gallbladder are both extremely rare. A partial or totally intrahepatic gallbladder is associated with an increased incidence of cholelithiasis.
Small ducts (of Luschka) may drain directly from the liver into the body of the gallbladder. If present, but not recognized at the time of a cholecystectomy, a bile leak with the accumulation of bile (biloma) may occur in the abdomen. An accessory right hepatic duct occurs in about 5% of cases. Variations of how the common bile duct enters the duodenum are described in earlier, in the Bile Ducts section.
Anomalies of the hepatic artery and the cystic artery are quite common, occurring in as many as 50% of cases.5 In about 5% of cases, there are two right hepatic arteries, one from the common hepatic artery and the other from the superior mesenteric artery. In about 20% of patients, the right hepatic artery comes off the superior mesenteric artery. The right hepatic artery may course anterior to the common duct. The right hepatic artery may be vulnerable during surgical procedures, in particular when it runs parallel to the cystic duct or in the mesentery of the gallbladder. The cystic artery arises from the right hepatic artery in about 90% of cases, but may arise from the left hepatic, common hepatic, gastroduodenal, or superior mesenteric arteries (Fig. 32-4).
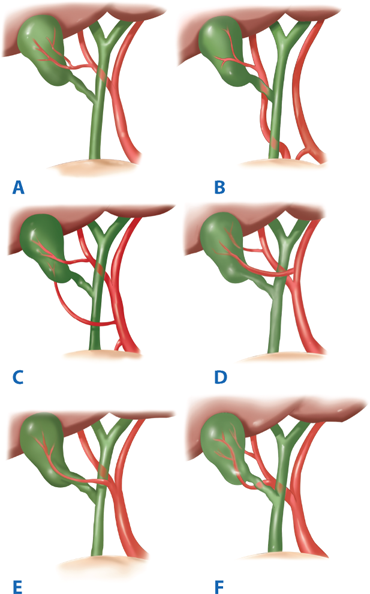
Figure 32-4.
Variations in the arterial supply to the gallbladder. A. Cystic artery from right hepatic artery, about 80% to 90%. B. Cystic artery from right hepatic artery (accessory or replaced) from superior mesenteric artery, about 10%. C. Two cystic arteries, one from the right hepatic, the other from the common hepatic artery, rare. D. Two cystic arteries, one from the right hepatic, the other from the left hepatic artery, rare. E. The cystic artery branching from the right hepatic artery and running anterior to the common hepatic duct, rare. F. Two cystic arteries arising from the right hepatic artery, rare.
PHYSIOLOGY
The liver produces bile continuously and excretes it into the bile canaliculi. The normal adult consuming an average diet produces within the liver 500 to 1000 mL of bile a day. The secretion of bile is responsive to neurogenic, humoral, and chemical stimuli. Vagal stimulation increases secretion of bile, whereas splanchnic nerve stimulation results in decreased bile flow. Hydrochloric acid, partly digested proteins, and fatty acids in the duodenum stimulate the release of secretin from the duodenum that, in turn, increases bile production and bile flow. Bile flows from the liver through to the hepatic ducts, into the common hepatic duct, through the common bile duct, and finally into the duodenum. With an intact sphincter of Oddi, bile flow is directed into the gallbladder.
Bile is mainly composed of water, electrolytes, bile salts, proteins, lipids, and bile pigments. Sodium, potassium, calcium, and chlorine have the same concentration in bile as in plasma or extracellular fluid. The pH of hepatic bile is usually neutral or slightly alkaline, but varies with diet; an increase in protein shifts the bile to a more acidic pH. The primary bile salts, cholate and chenodeoxycholate, are synthesized in the liver from cholesterol. They are conjugated there with taurine and glycine and act within the bile as anions (bile acids) that are balanced by sodium. Bile salts are excreted into the bile by the hepatocyte and aid in the digestion and absorption of fats in the intestines.6 In the intestines, about 80% of the conjugated bile acids are absorbed in the terminal ileum. The remainder is dehydroxylated (deconjugated) by gut bacteria, forming secondary bile acids deoxycholate and lithocholate. These are absorbed in the colon, transported to the liver, conjugated, and secreted into the bile. Eventually, about 95% of the bile acid pool is reabsorbed and returned via the portal venous system to the liver, the so-called enterohepatic circulation. Five percent is excreted in the stool, leaving the relatively small amount of bile acids to have maximum effect.
Cholesterol and phospholipids synthesized in the liver are the principal lipids found in bile. The synthesis of phospholipids and cholesterol by the liver is, in part, regulated by bile acids. The color of the bile is due to the presence of the pigment bilirubin diglucuronide, which is the metabolic product from the breakdown of hemoglobin and is present in bile in concentrations 100 times greater than in plasma. Once in the intestine, bacteria convert it into urobilinogen, a small fraction of which is absorbed and secreted into the bile.
The gallbladder, the bile ducts, and the sphincter of Oddi act together to store and regulate the flow of bile. The main function of the gallbladder is to concentrate and store hepatic bile and to deliver bile into the duodenum in response to a meal.
In the fasting state, approximately 80% of the bile secreted by the liver is stored in the gallbladder. This storage is made possible because of the remarkable absorptive capacity of the gallbladder, as the gallbladder mucosa has the greatest absorptive power per unit area of any structure in the body. It rapidly absorbs sodium, chloride, and water against significant concentration gradients, concentrating the bile as much as 10-fold and leading to a marked change in bile composition. This rapid absorption is one of the mechanisms that prevent a rise in pressure within the biliary system under normal circumstances. Gradual relaxation as well as emptying of the gallbladder during the fasting period also plays a role in maintaining a relatively low intraluminal pressure in the biliary tree.
The epithelial cells of the gallbladder secrete at least two important products into the gallbladder lumen: glycoproteins and hydrogen ions. The mucosal glands in the infundibulum and the neck of the gallbladder secrete mucus glycoproteins that are believed to protect the mucosa from the lytic action of bile and to facilitate the passage of bile through the cystic duct. This mucus makes up the colorless “white bile” seen in hydrops of the gallbladder resulting from cystic duct obstruction. The transport of hydrogen ions by the gallbladder epithelium leads to a decrease in the gallbladder bile pH. The acidification promotes calcium solubility, thereby preventing its precipitation as calcium salts.6
Gallbladder filling is facilitated by tonic contraction of the sphincter of Oddi, which creates a pressure gradient between the bile ducts and the gallbladder. During fasting, the gallbladder does not simply fill passively. In association with phase II of the interdigestive migrating myenteric motor complex in the gut, the gallbladder repeatedly empties small volumes of bile into the duodenum. This process is mediated at least in part by the hormone motilin. In response to a meal, the gallbladder empties by a coordinated motor response of gallbladder contraction and sphincter of Oddi relaxation. One of the main stimuli to gallbladder emptying is the hormone cholecystokinin (CCK). CCK is released endogenously from the duodenal mucosa in response to a meal.7 When stimulated by eating, the gallbladder empties 50% to 70% of its contents within 30 to 40 minutes. Over the following 60 to 90 minutes, the gallbladder gradually refills. This is correlated with a reduced CCK level. Other hormonal and neural pathways also are involved in the coordinated action of the gallbladder and the sphincter of Oddi. Defects in the motor activity of the gallbladder are thought to play a role in cholesterol nucleation and gallstone formation.8
The vagus nerve stimulates contraction of the gallbladder, and splanchnic sympathetic stimulation is inhibitory to its motor activity. Parasympathomimetic drugs contract the gallbladder, whereas atropine leads to relaxation. Neurally mediated reflexes link the sphincter of Oddi with the gallbladder, stomach, and duodenum to coordinate the flow of bile into the duodenum. Antral distention of the stomach causes both gallbladder contraction and relaxation of the sphincter of Oddi.
Hormonal receptors are located on the smooth muscles, vessels, nerves, and epithelium of the gallbladder. CCK is a peptide that comes from epithelial cells of the upper GI tract and is found in the highest concentrations in the duodenum. CCK is released into the bloodstream by acid, fat, and amino acids in the duodenum.9 CCK has a plasma half-life of 2 to 3 minutes and is metabolized by both the liver and the kidneys. CCK acts directly on smooth muscle receptors of the gallbladder and stimulates gallbladder contraction. It also relaxes the terminal bile duct, the sphincter of Oddi, and the duodenum. CCK stimulation of the gallbladder and the biliary tree also is mediated by cholinergic vagal neurons. In patients who have had a vagotomy, the response to CCK stimulation is diminished and the size and the volume of the gallbladder are increased.
Vasoactive intestinal polypeptide inhibits contraction and causes gallbladder relaxation. Somatostatin and its analogues are potent inhibitors of gallbladder contraction. Patients treated with somatostatin analogues and those with somatostatinoma have a high incidence of gallstones, presumably due to the inhibition of gallbladder contraction and emptying. Other hormones such as substance P and enkephalin affect gallbladder motility, but the physiologic role is unclear.7
The sphincter of Oddi regulates flow of bile (and pancreatic juice) into the duodenum, prevents the regurgitation of duodenal contents into the biliary tree, and diverts bile into the gallbladder. It is a complex structure that is functionally independent from the duodenal musculature and creates a high-pressure zone between the bile duct and the duodenum. The sphincter of Oddi is about 4 to 6 mm in length and has a basal resting pressure of about 13 mmHg above the duodenal pressure. On manometry, the sphincter shows phasic contractions with a frequency of about four per minute and an amplitude of 12 to 140 mmHg.8 The spontaneous motility of the sphincter of Oddi is regulated by the interstitial cells of Cajal through intrinsic and extrinsic inputs from hormones and neurons acting on the smooth muscle cells.10 Relaxation occurs with a rise in CCK, leading to diminished amplitude of phasic contractions and reduced basal pressure, allowing increased flow of bile into the duodenum (Fig. 32-5). During fasting, the sphincter of Oddi activity is coordinated with the periodic partial gallbladder emptying and an increase in bile flow that occurs during phase II of the migrating myoelectric motor complexes.11
DIAGNOSTIC STUDIES
A variety of diagnostic modalities are available for the patient with suspected disease of the gallbladder and the bile ducts. In 1924, the diagnosis of gallstones was improved significantly by the introduction of oral cholecystography by Graham and Cole. For decades, it was the mainstay of investigation for gallstones. In the 1950s, biliary scintigraphy was developed, as well as intrahepatic and endoscopic retrograde cholangiography (ERC), allowing imaging of the biliary tract. Later ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI) vastly improved the ability to image the biliary tract.12
When patients with suspected diseases of the gallbladder or the extrahepatic biliary tree are evaluated, a complete blood count and liver function tests are routinely requested. An elevated white blood cell (WBC) count may indicate or raise suspicion of cholecystitis. If associated with an elevation of bilirubin, alkaline phosphatase, and aminotransferase, cholangitis should be suspected. Cholestasis, an obstruction to bile flow, is characterized by an elevation of bilirubin (i.e., the conjugated form) and a rise in alkaline phosphatase. Serum aminotransferases may be normal or mildly elevated. In patients with biliary colic or chronic cholecystitis, blood tests will typically be normal.
An ultrasound is the initial investigation of any patient suspected of disease of the biliary tree.13 It is noninvasive, painless, does not submit the patient to radiation, and can be performed on critically ill patients. It is dependent upon the skills and the experience of the operator, and it is dynamic (i.e., static images do not give the same information as those obtained during the ultrasound investigation itself). Adjacent organs can frequently be examined at the same time. Obese patients, patients with ascites, and patients with distended bowel may be difficult to examine satisfactorily with an ultrasound.
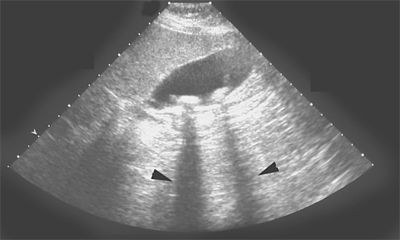
Ultrasound will show stones in the gallbladder with sensitivity and specificity of >90%. Stones are acoustically dense and reflect the ultrasound waves back to the ultrasonic transducer. Because stones block the passage of sound waves to the region behind them, they also produce an acoustic shadow (Fig. 32-6). Stones move with changes in position. Polyps may be calcified and reflect shadows, but do not move with change in posture. Some stones form a layer in the gallbladder; others a sediment or sludge. A thickened gallbladder wall and local tenderness indicate cholecystitis. The patient has acute cholecystitis if a layer of edema is seen within the wall of the gallbladder or between the gallbladder and the liver in association with localized tenderness. When a stone obstructs the neck of the gallbladder, the gallbladder may become very large, but thin walled. A contracted, thick-walled gallbladder is indicative of chronic cholecystitis.
The extrahepatic bile ducts are also well visualized by ultrasound, except for the retroduodenal portion. Dilation of the ducts in a patient with jaundice establishes an extrahepatic obstruction as a cause for the jaundice. Frequently, the site and, sometimes, the cause of obstruction can be determined by ultrasound. Small stones in the common bile duct frequently get lodged at the distal end of it, behind the duodenum, and are, therefore, difficult to detect. A dilated common bile duct on ultrasound, small stones in the gallbladder, and the clinical presentation allow one to assume that a stone or stones are causing the obstruction. Periampullary tumors can be difficult to diagnose on ultrasound, but beyond the retroduodenal portion, the level of obstruction and the cause may be visualized quite well. Ultrasound can be helpful in evaluating tumor invasion and flow in the portal vein, an important guideline for resectability of periampullary and pancreatic head tumors.14
Once considered the diagnostic procedure of choice for gallstones, oral cholecystography has largely been replaced by ultrasonography. It involves oral administration of a radiopaque compound that is absorbed, excreted by the liver, and passed into the gallbladder. Stones are noted on a film as filling defects in a visualized, opacified gallbladder. Oral cholecystography is of no value in patients with intestinal malabsorption, vomiting, obstructive jaundice, and hepatic failure.
Biliary scintigraphy provides a noninvasive evaluation of the liver, gallbladder, bile ducts, and duodenum with both anatomic and functional information. 99mTechnetium-labeled derivatives of dimethyl iminodiacetic acid (HIDA) are injected intravenously, cleared by the Kupffer cells in the liver, and excreted in the bile. Uptake by the liver is detected within 10 minutes, and the gallbladder, the bile ducts, and the duodenum are visualized within 60 minutes in fasting subjects. The primary use of biliary scintigraphy is in the diagnosis of acute cholecystitis, which appears as a nonvisualized gallbladder, with prompt filling of the common bile duct and duodenum. Evidence of cystic duct obstruction on biliary scintigraphy is highly diagnostic for acute cholecystitis. The sensitivity and specificity for the diagnosis are about 95% each. False-positive results are increased in patients with gallbladder stasis, as in critically ill patients and in patients receiving parenteral nutrition. Filling of the gallbladder and common bile duct with delayed or absent filling of the duodenum indicates an obstruction at the ampulla. Biliary leaks as a complication of surgery of the gallbladder or the biliary tree can be confirmed and frequently localized by biliary scintigraphy.15
Abdominal CT scans are inferior to ultrasonography in diagnosing gallstones. The major application of CT scans is to define the course and status of the extrahepatic biliary tree and adjacent structures. It is the test of choice in evaluating the patient with suspected malignancy of the gallbladder, the extrahepatic biliary system, or nearby organs, in particular, the head of the pancreas. Use of CT scan is an integral part of the differential diagnosis of obstructive jaundice (Fig. 32-7). Spiral CT scanning provides additional staging information, including vascular involvement in patients with periampullary tumors.16
Figure 32-7.
Computed tomography scan of the upper abdomen from a patient with cancer of the distal common bile duct. The cancer obstructs the common bile duct as well as the pancreatic duct. 1 = the portal vein; 2 = a dilated intrahepatic bile duct; 3 = dilated cystic duct and the neck of the gallbladder; 4 = dilated common hepatic duct; 5 = the bifurcation of the common hepatic artery into the gastroduodenal artery and the proper hepatic artery; 6 = dilated pancreatic duct; 7 = the splenic vein.
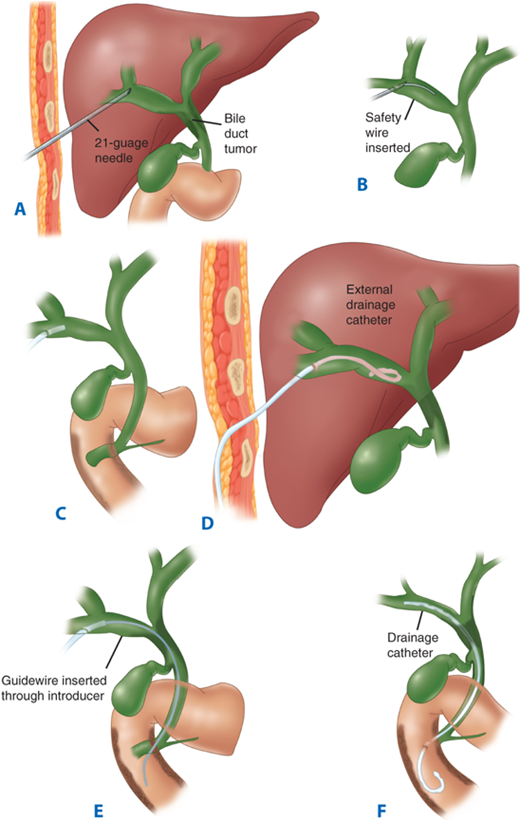
Intrahepatic bile ducts are accessed percutaneously with a small needle under fluoroscopic guidance. Once the position in a bile duct has been confirmed, a guidewire is passed, and subsequently, a catheter is passed over the wire (Fig. 32-8). Through the catheter, a cholangiogram can be performed and therapeutic interventions done, such as biliary drain insertions and stent placements. Percutaneous transhepatic cholangiography (PTC) has little role in the management of patients with uncomplicated gallstone disease but is particularly useful in patients with bile duct strictures and tumors, as it defines the anatomy of the biliary tree proximal to the affected segment. As with any invasive procedure, there are potential risks. For PTC, these are mainly bleeding, cholangitis, bile leak, and other catheter-related problems.15
Figure 32-8.
Schematic diagram of percutaneous transhepatic cholangiogram and drainage for obstructing proximal cholangiocarcinoma. A. Dilated intrahepatic bile duct is entered percutaneously with a fine needle. B. Small guidewire is passed through the needle into the duct. C. A plastic catheter has been passed over the wire, and the wire is subsequently removed. A cholangiogram is performed through the catheter. D. An external drainage catheter in place. E. Long wire placed via the catheter and advanced past the tumor and into the duodenum. F. Internal stent has been placed through the tumor.
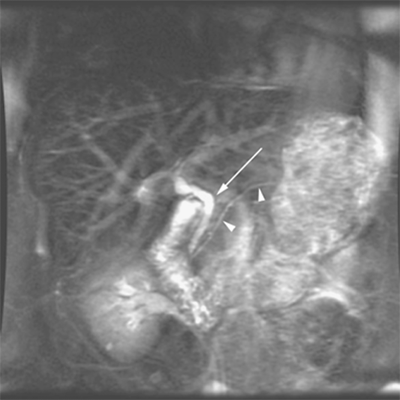
Available since the mid-1990s, MRI provides anatomic details of the liver, gallbladder, and pancreas similar to those obtained from CT. Many MRI techniques (i.e., heavily T2-weighted sequences, pulse sequences with or without contrast materials) can generate high-resolution anatomic images of the biliary tree and the pancreatic duct. It has a sensitivity and specificity of 95% and 89%, respectively, at detecting choledocholithiasis.17 MRI with magnetic resonance cholangiopancreatography (MRCP) offers a single noninvasive test for the diagnosis of biliary tract and pancreatic disease18 (Fig. 32-9). In many centers, MRCP is first performed for diagnosis of biliary and pancreatic duct pathology, reserving endoscopic retrograde cholangiopancreatography (ERCP) for therapeutic purposes only.
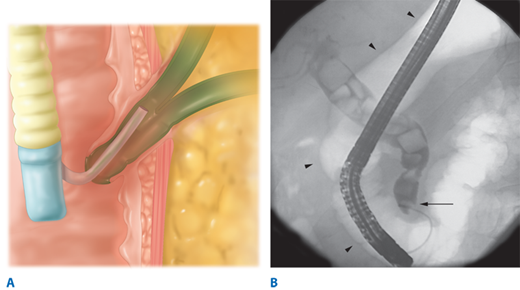
Using a side-viewing endoscope, the common bile duct can be cannulated and a cholangiogram performed using fluoroscopy (Fig. 32-10). The procedure requires intravenous (IV) sedation for the patient. The advantages of ERC include direct visualization of the ampullary region and direct access to the distal common bile duct, with the possibility of therapeutic intervention. The test is rarely needed for uncomplicated gallstone disease, but for stones in the common bile duct, in particular, when associated with obstructive jaundice, cholangitis, or gallstone pancreatitis, ERC is the diagnostic and often therapeutic procedure of choice. Once the endoscopic cholangiogram has shown ductal stones, sphincterotomy and stone extraction can be performed, and the common bile duct cleared of stones. In the hands of experts, the success rate of common bile duct cannulation and cholangiography is >90%. Complications of diagnostic ERC include pancreatitis and cholangitis and occur in up to 5% of patients.19 The development of small fiber-optic cameras that can be threaded through endoscopes used for endoscopic retrograde cholangiopancreatography (ERCP) has facilitated the development of intraductal endoscopy. By providing direct visualization of the biliary and pancreatic ducts, this technology has been shown to increase the effectiveness of ERCP in the diagnosis of certain biliary and pancreatic diseases.20,21 Intraductal endoscopy has been shown to have therapeutic applications that include biliary stone lithotripsy and extraction in high-risk surgical patients.22 As with most endoscopic procedures, intraductal endoscopy generally is considered safe, but there are no large trials that specifically address this issue. Typical complications such as bile duct perforation, minor bleeding from sphincterotomy or lithotripsy, and cholangitis have been described.23 Further refinement of this technology will enhance ERCP as a diagnostic and therapeutic tool.
Figure 32-10.
Endoscopic retrograde cholangiography. A. A schematic picture showing the side-viewing endoscope in the duodenum and a catheter in the common bile duct. B. An endoscopic cholangiography showing stones in the common bile duct. The catheter has been placed in the ampulla of Vater (arrow). Note the duodenal shadow indicated with arrowheads.
Endoscopic ultrasound requires a special endoscope with an ultrasound transducer at its tip. The results are operator dependent, but offer noninvasive imaging of the bile ducts and adjacent structures. It is of particular value in the evaluation of tumors and their resectability. The ultrasound endoscope has a biopsy channel, allowing needle biopsies of a tumor under ultrasonic guidance. Endoscopic ultrasound also has been used to identify bile duct stones, and although it is less sensitive than ERC, the technique is less invasive as cannulation of the sphincter of Oddi is not necessary for diagnosis of choledocholithiasis.
GALLSTONE DISEASE
Gallstone disease is one of the most common problems affecting the digestive tract. Autopsy reports have shown a prevalence of gallstones from 11% to 36%.24 The prevalence of gallstones is related to many factors, including age, gender, and ethnic background. Certain conditions predispose to the development of gallstones. Obesity, pregnancy, dietary factors, Crohn’s disease, terminal ileal resection, gastric surgery, hereditary spherocytosis, sickle cell disease, and thalassemia are all associated with an increased risk of developing gallstones.8 Women are three times more likely to develop gallstones than men, and first-degree relatives of patients with gallstones have a twofold greater prevalence.25
Most patients will remain asymptomatic from their gallstones throughout life. For unknown reasons, some patients progress to a symptomatic stage, with biliary colic caused by a stone obstructing the cystic duct. Symptomatic gallstone disease may progress to complications related to the gallstones.26 These include acute cholecystitis, choledocholithiasis with or without cholangitis, gallstone pancreatitis, cholecystocholedochal fistula, cholecystoduodenal or cholecystoenteric fistula leading to gallstone ileus, and gallbladder carcinoma. Rarely, complication of gallstones is the presenting picture.
Gallstones in patients without biliary symptoms are commonly diagnosed incidentally on ultrasonography, CT scans, or abdominal radiography or at laparotomy. Several studies have examined the likelihood of developing biliary colic or developing significant complications of gallstone disease. Approximately 3% of asymptomatic individuals become symptomatic per year (i.e., develop biliary colic). Once symptomatic, patients tend to have recurring bouts of biliary colic. Complicated gallstone disease develops in 3% to 5% of symptomatic patients per year. Over a 20-year period, about two thirds of asymptomatic patients with gallstones remain symptom free.27
Because few patients develop complications without previous biliary symptoms, prophylactic cholecystectomy in asymptomatic persons with gallstones is rarely indicated. For elderly patients with diabetes, for individuals who will be isolated from medical care for extended periods of time, and in populations with increased risk of gallbladder cancer, a prophylactic cholecystectomy may be advisable. Porcelain gallbladder, a rare premalignant condition in which the wall of the gallbladder becomes calcified, is an absolute indication for cholecystectomy.
Gallstones form as a result of solids settling out of solution. The major organic solutes in bile are bilirubin, bile salts, phospholipids, and cholesterol. Gallstones are classified by their cholesterol content as either cholesterol stones or pigment stones. Pigment stones can be further classified as either black or brown. In Western countries, about 80% of gallstones are cholesterol stones and about 15% to 20% are black pigment stones.28 Brown pigment stones account for only a small percentage. Both types of pigment stones are more common in Asia.
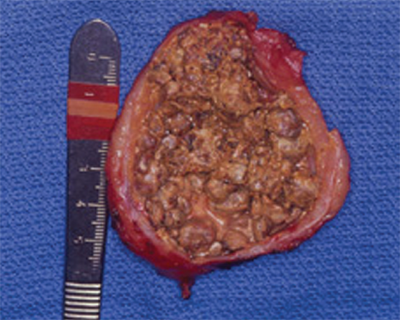
Pure cholesterol stones are uncommon and account for <10% of all stones. They usually occur as single large stones with smooth surfaces. Most other cholesterol stones contain variable amounts of bile pigments and calcium, but are always >70% cholesterol by weight. These stones are usually multiple, of variable size, and may be hard and faceted or irregular, mulberry-shaped, and soft (Fig. 32-11). Colors range from whitish yellow and green to black. Most cholesterol stones are radiolucent; <10% are radiopaque. Whether pure or of mixed nature, the common primary event in the formation of cholesterol stones is supersaturation of bile with cholesterol. Therefore, high bile cholesterol levels and cholesterol gallstones are considered as one disease. Cholesterol is highly nonpolar and insoluble in water and bile. Cholesterol solubility depends on the relative concentration of cholesterol, bile salts, and lecithin (the main phospholipid in bile). Supersaturation almost always is caused by cholesterol hypersecretion rather than by a reduced secretion of phospholipid or bile salts.2
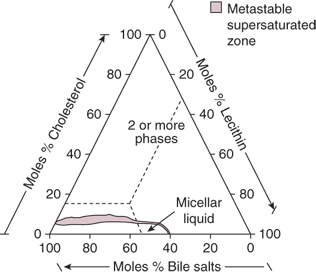
Cholesterol is secreted into bile as cholesterol-phospholipid vesicles. Cholesterol is held in solution by micelles, a conjugated bile salt-phospholipid-cholesterol complex, as well as by the cholesterol-phospholipid vesicles. The presence of vesicles and micelles in the same aqueous compartment allows the movement of lipids between the two. Vesicular maturation occurs when vesicular lipids are incorporated into micelles. Vesicular phospholipids are incorporated into micelles more readily than vesicular cholesterol. Therefore, vesicles may become enriched in cholesterol, become unstable, and then nucleate cholesterol crystals. In unsaturated bile, cholesterol enrichment of vesicles is inconsequential. In the supersaturated bile, cholesterol-dense zones develop on the surface of the cholesterol-enriched vesicles, leading to the appearance of cholesterol crystals. About one third of biliary cholesterol is transported in micelles, but the cholesterol-phospholipid vesicles carry the majority of biliary cholesterol29 (Fig. 32-12).
Figure 32-12.
The three major components of bile plotted on triangular coordinates. A given point represents the relative molar ratios of bile salts, lecithin, and cholesterol. The area labeled “micellar liquid” shows the range of concentrations found consistent with a clear micellar solution (single phase), where cholesterol is fully solubilized. The shaded area directly above this region corresponds to a metastable zone, supersaturated with cholesterol. Bile with a composition that falls above the shaded area has exceeded the solubilization capacity of cholesterol and precipitation of cholesterol crystals occurs. (Reproduced with permission from Holzbach RT. Pathogenesis and medical treatment of gallstones. In: Slesinger MH, Fordtran JS, eds. Gastrointestinal Diseases. Philadelphia: WB Saunders; 1989:1672.)
Pigment stones contain <20% cholesterol and are dark because of the presence of calcium bilirubinate. Otherwise, black and brown pigment stones have little in common and should be considered as separate entities.
Black pigment stones are usually small, brittle, black, and sometimes spiculated. They are formed by supersaturation of calcium bilirubinate, carbonate, and phosphate, most often secondary to hemolytic disorders such as hereditary spherocytosis and sickle cell disease, and in those with cirrhosis. Like cholesterol stones, they almost always form in the gallbladder. Unconjugated bilirubin is much less soluble than conjugated bilirubin in bile. Deconjugation of bilirubin occurs normally in bile at a slow rate. Excessive levels of conjugated bilirubin, as in hemolytic states, lead to an increased rate of production of unconjugated bilirubin. Cirrhosis may lead to increased secretion of unconjugated bilirubin. When altered conditions lead to increased levels of deconjugated bilirubin in bile, precipitation with calcium occurs. In Asian countries such as Japan, black stones account for a much higher percentage of gallstones than in the Western hemisphere.
Brown stones are usually <1 cm in diameter, brownish-yellow, soft, and often mushy. They may form either in the gallbladder or in the bile ducts, usually secondary to bacterial infection caused by bile stasis. Precipitated calcium bilirubinate and bacterial cell bodies compose the major part of the stone. Bacteria such as Escherichia coli secrete β-glucuronidase that enzymatically cleaves bilirubin glucuronide to produce the insoluble unconjugated bilirubin. It precipitates with calcium, and along with dead bacterial cell bodies, forms soft brown stones in the biliary tree.
Brown stones are typically found in the biliary tree of Asian populations and are associated with stasis secondary to parasite infection. In Western populations, brown stones occur as primary bile duct stones in patients with biliary strictures or other common bile duct stones that cause stasis and bacterial contamination.2,30
About two thirds of patients with gallstone disease present with chronic cholecystitis characterized by recurrent attacks of pain, often inaccurately labeled biliary colic. The pain develops when a stone obstructs the cystic duct, resulting in a progressive increase of tension in the gallbladder wall. The pathologic changes, which often do not correlate well with symptoms, vary from an apparently normal gallbladder with minor chronic inflammation in the mucosa, to a shrunken, nonfunctioning gallbladder with gross transmural fibrosis and adhesions to nearby structures. The mucosa is initially normal or hypertrophied, but later becomes atrophied, with the epithelium protruding into the muscle coat, leading to the formation of the so-called Aschoff-Rokitansky sinuses.
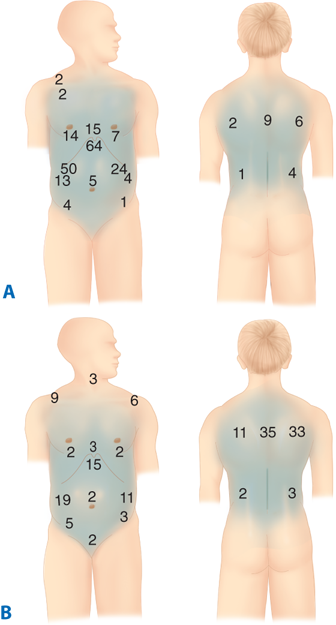
The chief symptom associated with symptomatic gallstones is pain. The pain is constant and increases in severity over the first half hour or so and typically lasts 1 to 5 hours. It is located in the epigastrium or right upper quadrant and frequently radiates to the right upper back or between the scapulae (Fig. 32-13). The pain is severe and comes on abruptly, typically during the night or after a fatty meal. It often is associated with nausea and sometimes vomiting. The pain is episodic. The patient suffers discrete attacks of pain, between which they feel well. Physical examination may reveal mild right upper quadrant tenderness during an episode of pain. If the patient is pain free, the physical examination is usually unremarkable. Laboratory values, such as WBC count and liver function tests, are usually normal in patients with uncomplicated gallstones.
Figure 32-13.
A. Sites of the most severe pain during an episode of biliary pain in 107 patients with gallstones (% values add up to >100% because of multiple responses). The subxiphoid and right subcostal areas were the most common sites; note that the left subcostal area was not an unusual site of pain. B. Sites of pain radiation (%) during an episode of biliary pain in the same group of patients. (Reprinted from Gunn A, Keddie N. Some clinical observations on patients with gallstones. Lancet. 1972;300(7771):239-241, Copyright 1972, with permission from Elsevier.)
Atypical presentation of gallstone disease is common. Association with meals is present in only about 50% of patients. Some patients report milder attacks of pain, but relate it to meals. The pain may be located primarily in the back or the left upper or lower right quadrant. Bloating and belching may be present and associated with the attacks of pain. In patients with atypical presentation, other conditions with upper abdominal pain should be sought out, even in the presence of gallstones. These include peptic ulcer disease, gastroesophageal reflux disease, abdominal wall hernias, irritable bowel disease, diverticular disease, liver diseases, renal calculi, pleuritic pain, and myocardial pain. Many patients with other conditions have gallstones.
When the pain lasts >24 hours, an impacted stone in the cystic duct or acute cholecystitis (see later Acute Cholecystitis section) should be suspected. An impacted stone without cholecystitis will result in what is called hydrops of the gallbladder. The bile gets absorbed, but the gallbladder epithelium continues to secrete mucus, and the gallbladder becomes distended with mucinous material. The gallbladder may be palpable but usually is not tender. Hydrops of the gallbladder may result in edema of the gallbladder wall, inflammation, infection, and perforation. Although hydrops may persist with few consequences, early cholecystectomy is generally indicated to avoid complications.
The diagnosis of symptomatic gallstones or chronic calculous cholecystitis depends on the presence of typical symptoms and the demonstration of stones on diagnostic imaging. An abdominal ultrasound is the standard diagnostic test for gallstones (see earlier Ultrasonography section).31 Gallstones are occasionally identified on abdominal radiographs or CT scans. In these cases, if the patient has typical symptoms, an ultrasound of the gallbladder and the biliary tree should be added before surgical intervention. Stones diagnosed incidentally in patients without symptoms should be left in place as discussed previously in the Natural History section. Occasionally, patients with typical attacks of biliary pain have no evidence of stones on ultrasonography. Sometimes only sludge in the gallbladder is demonstrated on ultrasonography. If the patient has recurrent attacks of typical biliary pain and sludge is detected on two or more occasions, cholecystectomy is warranted. In addition to sludge and stones, cholesterolosis and adenomyomatosis of the gallbladder may cause typical biliary symptoms and may be detected on ultrasonography. Cholesterolosis is caused by the accumulation of cholesterol in macrophages in the gallbladder mucosa, either locally or as polyps. It produces the classic macroscopic appearance of a “strawberry gallbladder.” Adenomyomatosis or cholecystitis glandularis proliferans is characterized on microscopy by hypertrophic smooth muscle bundles and by the ingrowths of mucosal glands into the muscle layer (epithelial sinus formation). Granulomatous polyps develop in the lumen at the fundus, and the gallbladder wall is thickened and septae or strictures may be seen in the gallbladder. In symptomatic patients, cholecystectomy is the treatment of choice for patients with these conditions.32
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree