Extramammary Paget Disease
Elsa F. Velazquez, MD
Key Facts
Terminology
Extramammary Paget disease (EMPD)
Clinical Issues
Erythematous patches or plaques with sharply defined borders
May clinically mimic chronic eczema
Microscopic Pathology
Round large pale cells in all levels of epidermis arranged as single units or confluent aggregates
Round vesicular nuclei with prominent nucleoli
Abundant clear cytoplasm
Absence of intercellular bridges
Paget cells often extend to adnexal structures
Flattened basal keratinocytes
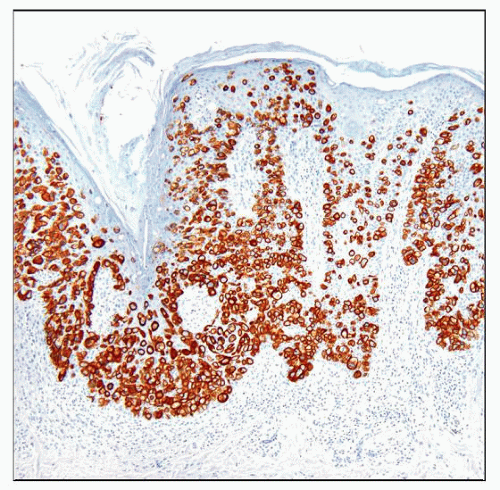
Ancillary Tests
Paget cells positive for mucin
Primary EMPD positive for CK7 and negative for CK20
Secondary EMPD has more variable immunohistochemical profile
Secondary EMPD associated with urothelial carcinoma positive for CK7 and CK20
Secondary EMPD associated with anal/rectal carcinoma positive for CK20 and negative for CK7
Top Differential Diagnoses
Squamous cell carcinoma in situ
Melanoma in situ
Clear cell papulosis
Benign mucinous metaplasia of penis
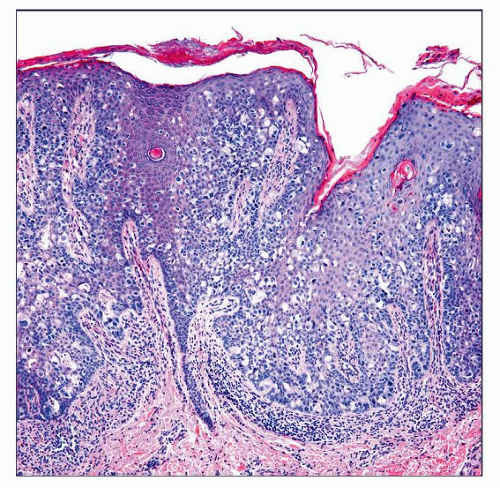 Large pale-staining neoplastic cells extensively infiltrate all levels of a hyperplastic epidermis in EMPD. There is a chronic inflammatory infiltrate in the upper dermis. |
TERMINOLOGY
Abbreviations
Extramammary Paget disease (EMPD)
Definitions
Adenocarcinoma involving epidermis and commonly extending to epithelium of eccrine glands &/or hair follicles (adenocarcinoma in situ)
May involve dermis in minority of cases
ETIOLOGY/PATHOGENESIS
Pathogenesis
Uncertain in most cases
Cases limited to epidermis are postulated to originate from intraepidermal portion of sweat glands or from intraepidermal stem cells
Heterogeneous condition; can be classified as primary (cutaneous origin) and secondary (extracutaneous origin)
Rarely, primary EMPD is associated with underlying sweat gland adenocarcinoma (usually apocrine)
Secondary EMPD may represent extension from urethral, bladder, anal/rectal, prostatic, or endocervical carcinoma
Incidence of association with internal carcinoma is about 15%
Especially true in perianal EMPD, which is associated with rectal carcinoma in 1/3 of cases
CLINICAL ISSUES
Epidemiology
Age
6th-8th decade
Gender
Female predominance
Site
Skin regions rich in apocrine glands
Most common sites are vulva and perianal region
Other sites include scrotum, perineum, penis, axilla, umbilicus
Exceptional sites include eyelid (accompanying carcinoma of Moll gland), external auditory meatus (associated with ceruminous carcinoma), face, scalp, chest, abdomen, and extremities
Presentation
Circinate or annular moist erythematous scaly patches or plaques
Gray-white eczematous patches are also common
Hypopigmented macules, ulceration, crusting, or palpable tumor may be present
Pruritus is frequent
Bleeding, oozing, tenderness, or burning sensation can occur
EMPD may mimic eczema
Lesions may be multifocal
Treatment
Complete surgical excision is treatment of choice for primary EMPD
Treatment in secondary lesions will depend on associated carcinoma
Prognosis
Primary EMPD confined to epidermis and epithelium of adnexal structures (in situ carcinoma) has good prognosis when completely excised
Patients require long-term follow-up because of multifocal nature of condition and high recurrence rate
Dermal invasion is associated with worse prognosis
Prognosis in secondary Paget disease is related to underlying carcinoma and is usually poor
MACROSCOPIC FEATURES
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree