Extended Cholecystectomy for Gallbladder Carcinoma
Prashant Khullar
Hisakazu Hoshi
The operations for gallbladder carcinoma have a wide range of variety from simple cholecystectomy for T1a cancer to extended right hepatectomy with regional nodal dissection for locally advanced disease. The standard operation for gallbladder cancer is a radical cholecystectomy, which involves resection of the gallbladder fossa which overlies segments IVb and V of the liver along with regional lymphadenectomy. However, involvement of the infundibulum and the cystic duct with cancer may require more extensive resections to include the bile duct and major hepatic resections to achieve negative resection margins.
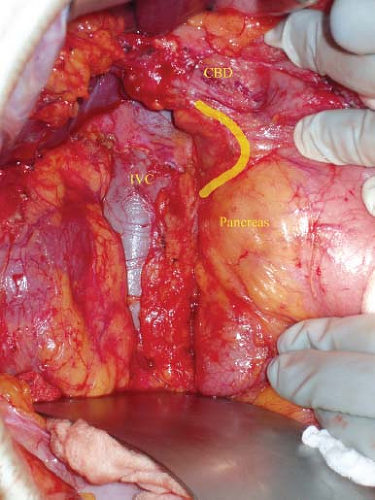
It is important to understand the pattern of the lymphatic drainage of gallbladder to perform a regional lymphadenectomy. The lymphatic channels from the gallbladder drain into the cystic and pericholedochal nodes first and subsequently can follow either of two pathways. Lymphatic channels can drain into the lower retroportal and retropancreatic nodes, and then to peri-SMA nodes (Fig. 74.1, yellow line) or to the proper hepatic artery nodes to common hepatic nodes and then to celiac axis nodes (Fig. 74.2, yellow line). However, the lymphatic dissemination of tumor cells is not always in an orderly fashion and skip metastases are common.
The operation should be modified depending on the clinical scenario in which gallbladder cancer presents. If the diagnosis is made on final pathologic examination after laparoscopic cholecystectomy and it is confined to the lamina propria (T1a), no additional operation may be necessary. For T1b or above, cystic duct stump excision, possible bile duct resection, regional lymphadenectomy, and liver resection are recommended for residual disease. On the other hand, extended resections including right hepatectomy, or right extended hepatectomy along with bile duct resection and reconstruction may be needed in case of locally advanced disease at initial presentation. Often times, intraoperative findings dictate the extent of the resection necessary to obtain R0 resection and the patient and surgeon should be prepared to take on this difficult task. Port site recurrences are regarded as stage IV disease and this category of patients may not derive any benefit from wide excision of port sites. The surgeon also has to keep in mind the variations in the origin of the hepatic artery, its branches and variations in bile duct anatomy.
SCORE™, the Surgical Council on Resident Education, classified operation for gallbladder cancer (when found incidentally) as an “ESSENTIAL UNCOMMON” procedure, and operation for gallbladder cancer (planned) as a “COMPLEX” procedure.
STEPS IN PROCEDURE
Bilateral subcostal incision or right subcostal incision with vertical extension up to the xiphoid process.
Abdominal exploration to look for locally advanced, unresectable disease or metastases.
Kocher maneuver to dissect posterior pancreaticoduodenal nodes and to sample aortocaval nodes.
Nodal dissection from celiac axis to the proper hepatic artery.
Identify aberrant arterial or bile duct anatomy.
Skeletonize porta hepatis to perform a portal lymphadenectomy. In case of prior hilar dissection or locally advanced disease, resection of the extrahepatic bile ducts may be required.
Assess for extent of hepatic resection depending on local extension of the disease.
Lower hilar plate by incising Glisson capsule at base of segment IVb.
Dissect inflow of segment IVb along the umbilical fissure.
Ensure low central venous pressure with anesthesiology assistance.
Pringle maneuver can be used intermittently to minimize blood loss.
Parenchymal division with appropriate device.
Identification and transection of middle hepatic vein with assistance of intraoperative ultrasound.
Identification and transection of segment V portal pedicle at the end of parenchymal transection.
HALLMARK ANATOMICAL COMPLICATIONS
Injury to portal vein, hepatic artery, or bile duct during portal dissection or hepatic parenchymal transection
Injury to middle hepatic vein during hepatic parenchymal transection
Parenchymal biliary leak
Postoperative bleeding or hematoma formation
Injury to duodenum or pancreas during portal lymphadenectomy
Aortic or caval injures during celiac or aortocaval lymph nodal dissection
LIST OF STRUCTURES
Gallbladder
Portal triad (portal vein, hepatic artery, common bile duct (CBD) and their branches)
Duodenum
Pancreas
Aorta
Inferior vena cava (IVC)
Left and right lobes of the liver
Ligamentum teres and umbilical fissure
Middle and right hepatic veins
Extended (Radical) Cholecystectomy
Abdominal Exploration and Assessment of Resectability
Technical Points
Position the patient supine on the table. A roll can be placed under the right side of patient’s torso to improve exposure. A right subcostal incision with an upward extension toward the xiphoid process provides adequate exposure to the relevant anatomy. Alternatively, a rooftop incision, or a vertical upper midline incision with a horizontal right lateral extension can
be made to provide a similar exposure. Perform a thorough abdominal exploration to rule out unresectable metastatic disease. Examine the liver by palpation. Use intraoperative ultrasound to identify vascular structures and lesions undetectable by preoperative radiologic imaging. Resectability of the tumor is also assessed by evaluating locoregional spread of the disease. Liver resection and a regional lymphadenectomy is the minimum operation required for any stage of gallbladder cancer beyond T1a. The extent of the tumor into the cystic duct will require resection of the bile duct and possibly an extended right hepatectomy for adequate margins.
be made to provide a similar exposure. Perform a thorough abdominal exploration to rule out unresectable metastatic disease. Examine the liver by palpation. Use intraoperative ultrasound to identify vascular structures and lesions undetectable by preoperative radiologic imaging. Resectability of the tumor is also assessed by evaluating locoregional spread of the disease. Liver resection and a regional lymphadenectomy is the minimum operation required for any stage of gallbladder cancer beyond T1a. The extent of the tumor into the cystic duct will require resection of the bile duct and possibly an extended right hepatectomy for adequate margins.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree