Esophagus: Diagnosis and Margins
SURGICAL/CLINICAL CONSIDERATIONS
Goal of Consultation
Determine whether proximal and distal margins are free of carcinoma and dysplasia
Change in Patient Management
Additional tissue at proximal or distal margin may be resected
Clinical Setting
Neoplasms of esophagus are frequently detected due to clinical symptoms
Surgery may be indicated for potential cure or palliation
Majority of lesions will have been diagnosed by endoscopic biopsy
Many carcinomas undergo preoperative chemotherapy or radiation therapy
Status of margins can be difficult to evaluate by frozen section for some lesions
Adenocarcinomas associated with Barrett mucosa and dysplasia
Diffusely invasive signet ring cell carcinomas of stomach
Carcinomas after treatment
SPECIMEN EVALUATION
Gross
Identify esophagus, stomach, and duodenum (if present in complete gastrectomy)
Examine outer surface for tumor involvement
Ink serosa and adventitia along area to be opened
For partial gastrectomies, margin can be marked with clips to aid in identification after opening
Open along greater curvature of stomach unless lesion is located at this site
Open stapled margins as close to staples as possible
Identify cancer site
Cancers above gastroesophageal (GE) junction are usually squamous cell carcinomas
Cancers at GE junction are usually adenocarcinomas
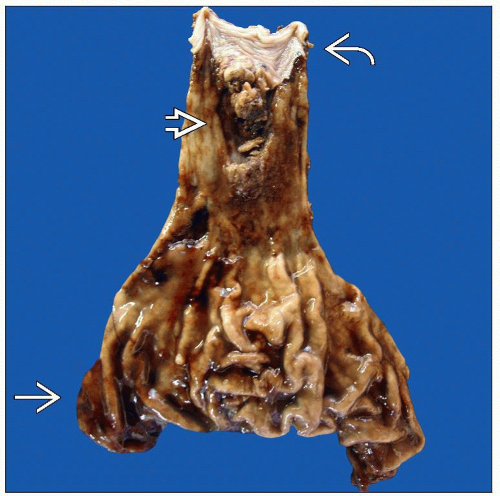
Often associated with Barrett mucosa; pink granular appearance
Cancers in stomach are usually adenocarcinomas
Majority present with ulcerated center and heapedup edges
Signet ring cell carcinomas may present as linitis plastica; muscularis propria is diffusely thickened; mucosal surface may appear normal
If there has been prior treatment, cancer site may be subtle area of ulceration or fibrosis
Measure distance of cancer or tumor bed to closest proximal and distal margins
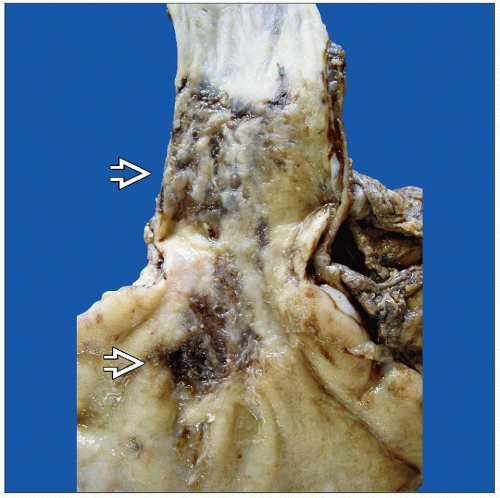
GE junction adenocarcinomas can invade under overlying normal squamous mucosa for 1-2 cm
Signet ring cell carcinomas can invade below overlying normal mucosa and in muscularis of stomach for several cm
Frozen Section
Section of closest margin to cancer is selected
Margin section must include full cross section of mucosa, submucosa, and muscularis propria
Mucosa can sometimes curl over at cut edge of specimen due to retraction of muscularis propria
It may be necessary to retract mucosa slightly to get a full-thickness section
Distal (gastric) margin is usually far from carcinoma
Representative section can be frozen but is rarely positive
In cases of signet ring cell carcinoma or other primary gastric carcinomas, more extensive evaluation of margin may be indicated
Margins can be taken en face (parallel to margin) or perpendicular to margin
MOST COMMON DIAGNOSES
Barrett Mucosa
Replacement of normal squamous mucosa of distal esophagus by abnormal glandular mucosa
May be patchy and discontinuous
Recognized by pale pink, finely granular tissue replacing normal white, smooth, and glistening squamous surface
Areas of high-grade dysplasia and small carcinomas may form small areas of heaped-up mucosa
Esophageal margin should be free of Barrett mucosa
Adenocarcinoma, Intestinal Type
Usually arise in distal esophagus in area of Barrett mucosa
Can be multifocal
Tan-pink masses with heaped-up borders and central ulceration are typical
Adenocarcinoma, Signet Ring Cell Type
Signet ring cell carcinomas are more common in stomach
Diffuse involvement of mucosa and muscularis can be difficult to detect grossly and on frozen section
Muscularis propria may be diffusely thickened (linitis plastica)
Signet ring cells can be difficult to distinguish from histiocytes or plasma cells
Squamous Cell Carcinoma
Arise at any level of esophagus
Can be multifocal
May be exophytic, ulcerating, or cause diffuse thickening and narrowing of lumen
Many will have been treated with preoperative radiation therapy
After treatment, tumor bed may be a subtle area of shallow ulceration or granular-appearing squamous mucosa
Radiation atypia may be difficult to distinguish from carcinoma in situ
Esophageal margin should be evaluated for squamous cell carcinoma in situ as well as for invasive carcinoma
Leiomyoma or Gastrointestinal Stromal Tumor (GIST)
Arise from muscularis
Well-circumscribed, pink to white masses with whorled appearance
Spindle cells grow in fascicles
GIST is rare in this location
Majority are malignant
Margins can be evaluated grossly
Granular Cell Tumor
Arise in submucosa or muscularis propria of distal esophagus
Abundant granular pink cytoplasm
Overlying mucosa is intact
Pseudoepitheliomatous hyperplasia can mimic squamous cell carcinoma
REPORTING
Frozen Section
Margins positive or negative for invasive carcinoma, carcinoma in situ, Barrett mucosa, or tumor bed
If carcinoma is close to margin, distance from margin is reported
PITFALLS
Carcinoma vs. Treatment-Related Changes
Many patients are treated with preoperative chemotherapy &/or radiation therapy
Carcinomas can be difficult to identify
Scattered atypical cells in fibrotic tumor bed
Cells can have marked cytoplasmic vacuolization
Mucin pools with scarce or absent tumor cells
Atypical changes in benign cells can mimic carcinoma
Squamous mucosa
Enlarged, irregular nuclei
Mitoses
Abundant vacuolated cytoplasm
Hyperkeratosis, acanthosis, parakeratosis
Glandular mucosa
Neuroendocrine cells are resistant to treatment and may form small clusters
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree