Esophageal Resection: Esophagogastrectomy and the Ivor Lewis Approach
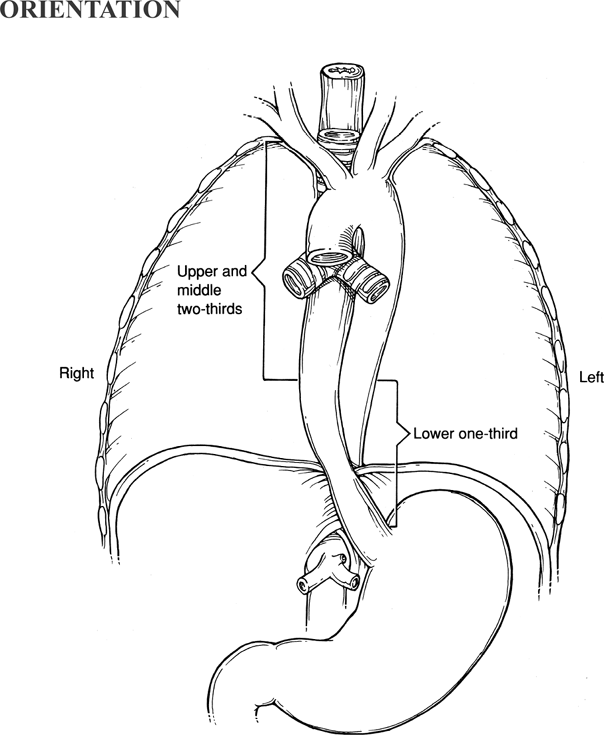
Lesions of the lower to middle third of the esophagus are approached through a thora-cotomy in conjunction with laparotomy. The lower esophagus is easily reached through the left chest, but the middle esophagus is inaccessible through this approach. Esophagogastrectomy (resection of the lower esophagus and upper stomach) is employed for carcinoma of the cardioesophageal junction. Lesions that extend above this level are better managed by an Ivor Lewis (laparotomy and right thoracotomy) type of resection, which provides access to the entire thoracic esophagus. Alternative surgical approaches, such as esophagectomy without thoracotomy and minimally invasive esophagectomy, are described in subsequent chapters and in the references.
Steps in Procedure
Esophagogastrectomy
Left thoracoabdominal incision (begin with abdominal portion and thorough exploration)
Mobilize stomach by creating window along greater curvature
Retain blood supply to greater and lesser curvature
Perform pyloromyotomy by creating incision across pylorus
Perform Kocher maneuver to mobilize duodenum
Reflect left lung upward and incise inferior pulmonary ligament to level of inferior pulmonary vein
Incise pleura overlying esophagus and develop flaps of pleura
Dissect tumor from mediastinum, taking adjacent lymph nodes with specimen
Place two stay sutures on proximal esophagus and divide it
Divide stomach with linear stapling device, 4.8 cartridge
Check hemostasis
Create gastrotomy and insert EEA stapler into stomach, bringing it out through anterior wall of proximal part of pouch
Place anvil in esophagus and secure with pursestring suture
Complete the stapled anastomosis
Reinforce the staple line by inkwelling the stomach over the anastomosis
Check hemostasis and place chest tubes
Close diaphragm with interrupted 3-0 figure-of-eight sutures
Tack stomach to hiatus
Pass nasogastric tube through anastomosis to region of pylorus and secure
Close thoracic and abdominal portion of incision in usual fashion
Ivor Lewis Resection
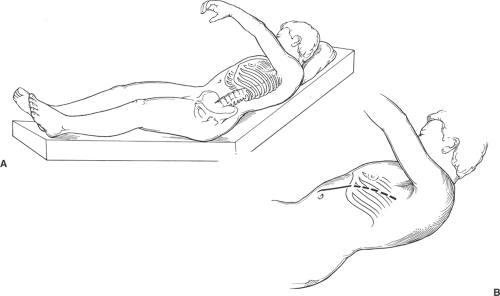
Supine position, hips flat, right chest elevated into thoracotomy position, right neck exposed
Upper midline incision, explore abdomen
Mobilize stomach as previously described
Right thoracotomy, 5th interspace
Incise pleura over esophagus
Identify azygos vein and incise overlying pleura, ligate and divide vein
Surround esophagus above tumor with Penrose drain
Carefully dissect tumor from mediastinum, including nodes with specimen
Decide whether to create anastomosis in chest or in neck
Anastomosis in Chest
Divide stomach with stapler
Place two stay sutures on proximal esophagus and divide it
Check mediastinum for hemostasis
Anastomosis and pass nasogastric tube as previously described
Tack stomach to parietal pleura
Place two chest tubes and close thoracotomy
Close laparotomy incision in usual fashion
Anastomosis in Neck
Expose cervical esophagus and mobilize it
Connect neck field with thoracotomy field by following esophagus down into chest
Divide esophagus in neck
Hand sew two-layer anastomosis of stomach to esophagus
Place two chest tubes and close thoracotomy
Place small Penrose drain in cervical incision and close incision
Close laparotomy incision without drainage
Hallmark Anatomic Complications
Injury to phrenic nerve (diaphragmatic incision)
Injury to azygos vein
Anastomotic leak
Injury to membranous portion of trachea
List of Structures
Esophagus
Diaphragm
Phrenic nerve
Internal Thoracic (Mammary) Artery
Musculophrenic artery
Superior epigastric artery
Rectus abdominis muscle
Inferior pulmonary ligament
Inferior pulmonary vein
Stomach
Pylorus
Cardia
Short gastric vessels
Spleen
Left gastroepiploic vessels
Right gastroepiploic vessels
Gastroduodenal artery
Gastrocolic ligament
Greater omentum
Lesser omentum
Right gastric artery
Left gastric artery
Coronary vein
Inferior phrenic artery
Aorta
Azygos vein
Thoracic duct
Internal jugular vein
Sternocleidomastoid muscle
Omohyoid muscle
Middle thyroid veins
Recurrent laryngeal nerve
 |
Esophagogastrectomy
Incision and Initial Exploration (Fig. 30.1)
Technical Points
Position the patient in a modified left thoracotomy position. Place the hips of the patient flat on the operating table. Raise the left shoulder and support the left arm. Ideally, the shoulders should be in an almost full thoracotomy position, while the pelvis is flat. Patients with less flexible spines may not be able to tolerate this position. In such cases, the patient’s pelvis should be allowed to rotate with the upper trunk.
Plan a thoracoabdominal incision that extends in a straight line from the eighth intercostal space to a point just above and slightly beyond the umbilicus. Mark the line of the proposed skin incision. Make your initial incision through just the abdominal portion of this incision and assess resectability of the tumor before proceeding into the chest.
Incise the fascial and muscular layers of the abdominal wall in a direct line with the incision. Use electrocautery to control bleeding as you pass through the muscular layers of the abdominal wall. Continue the skin incision up several centimeters over the costal margin, but do not yet divide the costal margin.
Assess resectability by palpating the tumor at the cardioesophageal junction and assessing its mobility. Check the liver and other intraabdominal viscera for metastatic deposits. Palpable nodes along the celiac axis do not necessarily preclude resection, which will provide the best palliation for a lesion in this area. If the lesion is believed to be resectable, extend the incision up into the chest. Divide the costal cartilage and excise a 1 cm piece of it. After opening the left chest in the eighth intercostal space and attaining hemostasis in the intercostal muscles, place a self-retaining or Finochietto-type retractor and spread the ribs.
Divide the diaphragm with a curvilinear lateral incision that is planned to avoid the phrenic nerve. Sharply divide the inferior pulmonary attachments and reflect the left lung upward. An indwelling nasogastric tube or esophageal stethoscope should be palpable in the esophagus.
Anatomic Points
When planning a thoracoabdominal incision, make sure that the thoracic part of the incision is through the appropriate intercostal space. The first rib cannot be palpated because of the clavicle; hence, one must start counting with the second rib, which articulates with the sternum at the sternal angle of Lewis. The incision should be inferior to the pectoralis major and minor muscles. As in any thoracic incision, divide the intercostal muscles along the superior margin of the lower rib to avoid the intercostal neurovascular bundle. Remember that the anterior portion of the costal margin is formed by the union of costal cartilages of the eighth through tenth ribs articulating with the cartilage of the rib above, and that the lowest costal cartilage articulating with the sternum is that of the seventh rib.
The combined thoracoabdominal incision divides the terminal branches of the internal thoracic (mammary) artery. One of these branches—the musculophrenic artery—passes inferolaterally behind the seventh to ninth costal cartilages. The other—the superior epigastric artery—is divided when the rectus abdominis muscle is divided. Both arteries have free anastomoses with other arteries.
Division of the diaphragm must take into account the location of the phrenic nerve and its three major branches. The left phrenic nerve enters the muscular part of the right hemidiaphragm just lateral to the left cardiac surface. As it traverses the diaphragm, it divides into a sternal branch that runs anteromedially toward the sternum, an anterolateral branch that passes laterally anterior to the central tendon, and a posterior branch that runs posterior to the central tendon and that supplies crural fibers to the left of the esophageal hiatus, regardless of whether the esophageal hiatus is entirely surrounded by right crus or by both left and right crura.
The mediastinal root of the pulmonary ligament is anterior to the esophagus. Division of this ligament allows the lung to be retracted superiorly, exposing the distal esophagus in the left chest. Caution must be exercised, however, because the fragile inferior pulmonary vein lies at the top of the pulmonary ligament.
Mobilization of the Stomach and Pyloromyotomy (Fig. 30.2)
Technical Points
Mobilize the stomach by creating a window along the greater curvature. The spleen may be taken with the specimen. The mobilization is essentially the same as that described for total gastrectomy (see Chapter 53). Preservation of the omentum will allow some omentum to be wrapped around the anastomosis at the conclusion of the surgery, thus ensuring a good blood supply for the stomach. Fully mobilize the stomach from the pylorus to the cardioesophageal junction.
Perform a Kocher maneuver to mobilize the duodenum. Do this by incising the peritoneum lateral to the duodenum and elevating the duodenum off the retroperitoneum by sharp and blunt dissection. This should be an avascular plane that allows the duodenum to rotate toward the midline. The head of the pancreas will come up with the duodenum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree