Eosinophilia
Carla S. Wilson, MD, PhD
Key Facts
Terminology
Absolute eosinophil count > 0.5 × 109/L, independent of age
Etiology/Pathogenesis
Reactive eosinophilia is usually caused by eosinopoietic cytokines, primarily IL-5 and GM-CSF
In industrialized countries allergens are most common cause of eosinophilia
In hospitalized patients medications are most common cause
In nonindustrialized countries parasites are most common cause
Activated eosinophils release proinflammatory mediators that cause tissue damage
Intravascular degranulation of eosinophils causes
Generalized endothelial damage
Endomyocardial fibrosis
Marked propensity for thrombus formation
Clinical Issues
Initial evaluation requires detailed history, physical examination, complete blood count, and blood film evaluation
Microscopic Pathology
Eosinophil atypia may be seen in both reactive and neoplastic disorders
Bone marrow is often normocellular unless associated with an autoimmune or neoplastic disorder
Top Differential Diagnoses
Idiopathic hypereosinophilic syndrome (HES)
Eosinophil count > 1.5 × 109/L for > 6 months
No tissue damage
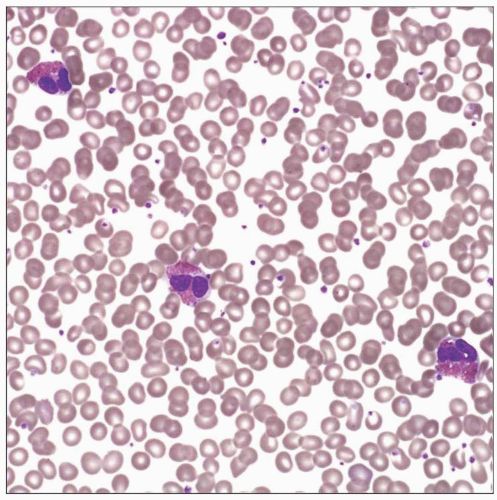
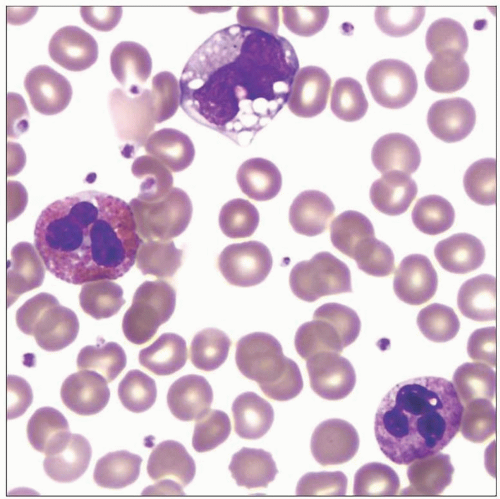 Mature eosinophils are 10-15 um in size. The cytoplasmic, orange-red, refractile granules most easily distinguish the eosinophil in this image from the monocyte and neutrophil. |
TERMINOLOGY
Synonyms
Increased eosinophils
Reactive eosinophilia
Secondary eosinophilia
Eosinophilic hyperplasia
Absolute eosinophilia
Definitions
Absolute eosinophil count > 0.5 × 109/L, independent of age
Arbitrary ranges include
Mild (0.6-1.5 × 109/L)
Moderate (1.6-5.0 × 109/L)
Severe (> 5 × 109/L)
ETIOLOGY/PATHOGENESIS
Environmental Exposure
Allergies
Asthma
Hayfever
Allergic rhinitis
Sinusitis
Drug hypersensitivity
Numerous drugs
Recombinant cytokine therapy
Infectious Agents
Parasites: Helminths
Ascariasis
Hookworm
Filariasis
Schistosomiasis
Trichinosis
Strongyloidiasis
Cysticercosis
Echinococcosis
Paragonimiasis
Toxocariasis
Visceral larva migrans
Fungal
Cryptococcosis
Aspergillosis
Coccidioidomycosis
Histoplasmosis
Blastomycosis
Protozoal
Isospora belli
Dientamoeba fragilis
Bacterial
Viral
Human T-cell lymphotrophic virus
West Nile virus
Underlying Illness
Pulmonary disorders
Loeffler syndrome
Hypersensitivity pneumonitis
Bronchiectasis
Pneumonia
Churg-Strauss syndrome
Skin lesions
Atopic dermatitis
Urticaria
Pemphigus
Bullous pemphigoid
Angiolymphoid hyperplasia
Wells syndrome
Eosinophilic panniculitis
Gastrointestinal disease
Celiac disease
Inflammatory bowel disease
Eosinophilic gastroenteritis
Chronic pancreatitis
Immunologic Disorders
Neoplastic Processes; Eosinophils Nonneoplastic
Classical Hodgkin lymphoma
T-cell lymphoproliferative disorders
B-lymphoblastic leukemia with t(5;14)(q31;q32) IL3-IGH@
Langerhans cell histiocytosis
Myelodysplastic syndromes
Aberrant T-cell population (T cells may or may not be clonal)
Natural killer (NK) cell neoplasms
Carcinoma (paraneoplastic syndrome associated)
Pathogenesis
Cytokine-producing constituents in secondary (reactive) eosinophilia
Activated T-cells (Th2)
Mast cells
Stromal cells
Various neoplastic cells (e.g., lymphoma cells)
Cytokines that stimulate eosinophil production in bone marrow
IL-5
IL-3
IL-2
GM-CSF
Sustained cytokine production linked to chronic eosinophilia
Constitutive IL-3 activation in B-lymphoblastic leukemia with t(5; 14) IL3-IGH@
Eosinophil maturation takes approximately 5 days
Eosinophils circulate 18-24 hours before migrating into tissues
Chemotactic factors recruit eosinophils from blood into tissue
Eotaxin
IL-5
Majority of eosinophils are in tissues
Activated eosinophils release proinflammatory mediators that cause tissue damage
Intravascular degranulation of eosinophils causes
Generalized endothelial damage
Endomyocardial fibrosis
Marked propensity for thrombus formation
In industrialized countries allergens are most common cause
In hospitalized patients medications are most common cause
In nonindustrialized countries parasites most common cause
CLINICAL ISSUES
Presentation
Transient eosinophilia: Acute reactive processes infections
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree