Endoscopic Parathyroidectomy by Lateral Approach
Jean-François Henry
DEFINITION
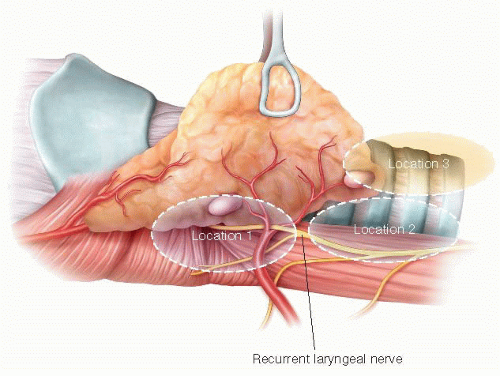
A minimally invasive parathyroidectomy (MIP) may be defined as an operation requiring a small and discrete incision for a very direct access to the parathyroid glands, resulting in a focused dissection. MIP may be divided in two groups: open MIP performed under direct vision via a small cervical incision1 and various endoscopic MIP performed partially or totally with the help of an endoscope. Today, three different types of endoscopic parathyroidectomies can be considered to be an option for surgeons: (1) Video-assisted parathyroidectomy,2 which is a mini-open procedure performed partially with the help of the endoscope. (2) Endoscopic techniques using an extracervical approach. These techniques have the advantage of leaving no scar in the neck area but cannot reasonably be described as minimally invasive as they require more dissection than conventional open surgery. (3) Pure endoscopic techniques using a cervical access. These operations are performed totally with the help of the endoscope and include constant gas insufflations. Two pure endoscopic techniques have been described: the endoscopic parathyroidectomy by midline approach3 and the endoscopic parathyroidectomy by lateral approach (EPLA).4 EPLA develops the plane between the carotid sheath laterally and the strap muscles medially. This “back-door route” does not require complete dissection of the thyroid lobe from the strap muscles. It allows direct access to the posterior aspect of the thyroid lobe and it does not require anterior and medial retraction of the thyroid lobe during the entire procedure.
DIFFERENTIAL DIAGNOSIS
Today, the diagnosis of primary hyperparathyroidism (PHPT) can be made with near certainty by documenting an increased serum intact parathormone (iPTH) level in a patient with increased ionized or total calcium. It is therefore necessary to eliminate all other causes of hypercalcemia and iPTH elevation. As for iPTH elevation, renal dysfunction and vitamin D deficiency are well known. Among causes of hypercalcemia, thought should be given to the syndrome of benign familial hypocalciuric hypercalcemia (BFHH), where the hypercalcemia is associated with normal or slightly raised levels of iPTH coexisting with hypocalciuria.
PATIENT HISTORY AND PHYSICAL FINDINGS
The patient must be carefully selected. Not all patients presenting with HPT are candidates for an EPLA, as EPLA does not allow for a bilateral exploration.5 Patients who are suspected to have multiglandular disease (MGD), including patients with secondary hyperparathyroidism (HPT) or patients with familial primary HPT, are not eligible for this procedure. Suspicion of parathyroid carcinoma is also an absolute contraindication. A history of neck irradiation, the presence of a large goiter and previous surgery in the thyroid vicinity are relative contraindications. EPLA can be performed in patients who have previously undergone a contralateral neck operation (Table 1).
When considering EPLA, the adenoma must be solitary and clearly localized by preoperative imaging studies. Whether preoperative localizations techniques can rule out MGD with sufficient accuracy is questionable. Therefore, as with other minimally invasive techniques, the risk of missing MGD justifies the use of a quick intraoperative parathormone assay (QPTH).6 The less definitive the localizations studies, the more imperative the need for QPTH.
When patients are selected on the basis of the abovementioned criteria, no more than 50% of patients are eligible for this procedure (FIG 1).
EPLA is technically more challenging than standard cervical exploration and its performance should be confined to tertiary centers. The surgeon must be experienced in conventional parathyroid surgery. Mentoring by a surgeon who has experience with endoscopic neck procedures is also recommended.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Only noninvasive tests should be considered. When these tests are negative, EPLA is not indicated and the traditional open cervicotomy is preferable. The topographic diagnosis should ideally be established by convergence of the results of two different investigations, one providing good anatomic information and the other providing functional information.
Table 1: Absolute and Relative Contraindications for Endoscopic Parathyroidectomy by Lateral Approach
Absolute contraindications
Suspicion of parathyroid carcinoma
Large goiter
Secondary or tertiary HPT
Familial HPT
Suspicion of MGD
No localization
Relative contraindications
Previous surgery
History of neck irradiation
Large tumor (>3 cm)
Inferior adenoma located anteriorly
HPT, hyperparathyroidism; MGD, multiglandular disease.
High-resolution ultrasonography (US) and technetium-99m (Tc-99m) sestamibi scan are used most commonly in combination.7 US can only assess the cervical region but gives good anatomic information, including useful information about the thyroid gland. The patient should be examined in the supine position with the neck in hyperextension. A pillow can be placed under the shoulders if the patient has a short neck. A high-frequency linear transducer
(7.5 to 10 MHz) is used to obtain optimal depth penetration of 3 to 4 cm. A bilateral and comparative scan should be performed in transverse section, then in longitudinal section. In transverse section, the examination concentrates on an area defined by the longus colli muscles posteriorly, the thyroid gland anteriorly, the trachea medially, and the carotid artery laterally. The scan is then performed in cranial and caudal directions. An additional scan can be performed with the head of the patient turned away to the side and during deglutition to optimize the lateroesophageal images. The anterosuperior mediastinum is examined by inclining the transducer deeply in a retrosternal direction. The examiner should note the precise location with respect to surrounding structures, particularly to the thyroid gland, and the depth from the skin. Finally, a color flow Doppler or a power flow Doppler will be performed to test the vascularization of the area and define the artery branches involved.
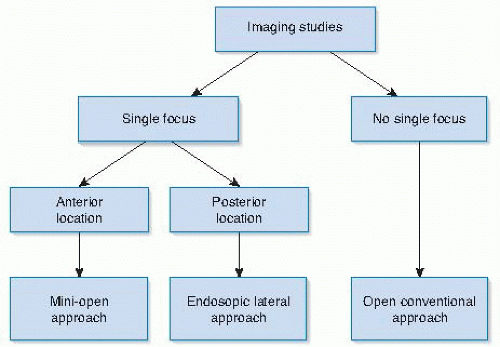
FIG 1 • Algorithm for the surgical management of patients eligible for an endoscopic parathyroidectomy by lateral approach.
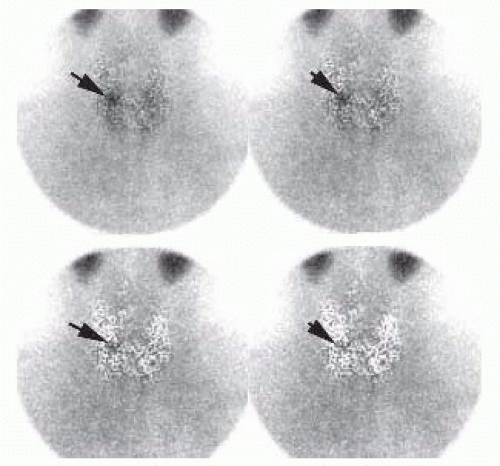
Two protocols for sestamibi scanning can be used: the single isotope dual phase protocol and the substraction protocol. The dual protocol requires early (15 minutes postinjection) and delayed images (at 1 and 2 to 3 hours, depending on thyroid washout). In cases of multinodular thyroid disease, additional further delayed images are sometimes needed. When a subtraction protocol is used, Tc-99m sestamibi is used in conjunction with another radionuclide specific to the thyroid. Tc-99m pertechnetate and123I are the most widely used radioisotopes for thyroid scintigraphy. The main advantage of using123I is that thyroid and parathyroid images can be acquired simultaneously in a dual energy window setup. The disadvantage is the cost of the protocol related to123I. Parathyroid scintigraphy should include views of the neck and the mediastinum. Single-photon emission computed tomography (SPECT) can be helpful for more precise localization of adenomas, as it provides simultaneous three-dimensional (3-D) information on both neck and superior mediastinum.
Instead of US and Tc-99m sestamibi scan, four-dimensional computed tomography (4D-CT)8 or the use of computed axial tomography-methoxyisobutyl isonitrile (MIBI) image fusion,9 when available, may be preferable.
Consideration for EPLA depends on the results of preoperative imaging. EPLA should be strongly considered when the parathyroid adenoma is in close proximity to the recurrent laryngeal nerve, as the nerve is at risk during MIP. Therefore, EPLA is the procedure of choice in all cases where the parathyroid adenomas are deeply located in the neck.
Three locations of parathyroid adenomas with regard to the recurrent laryngeal nerve can be described (FIG 2).4 Location 1 is posterior to the two superior thirds of the thyroid lobe (FIGS 3 and 4). These adenomas are superior glands. Location 2 is at the level of or below the inferior pole of the thyroid lobe but in a plane posterior to it (FIGS 5 and 6). These adenomas may be either a superior gland that has migrated posteriorly and in a downward direction or an inferior gland that has fallen posteriorly. These glands can also migrate into the superior and posterior mediastinum. Location 3 is at the level of or below the inferior pole of the thyroid lobe but in a superficial plane (FIGS 7 and 8). These adenomas are always inferior glands and can be found in close contact with the tip of the inferior pole of the thyroid lobe but also along the thyrothymic ligament or into the superior pole of the thymus.
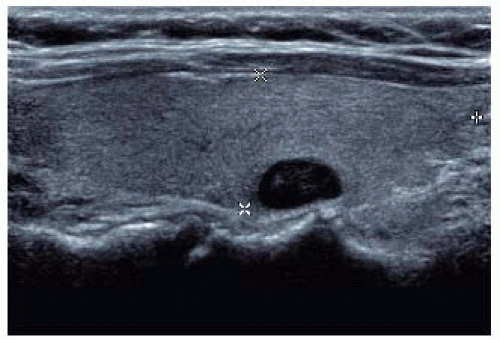
FIG 4 • Ultrasound (same patient in FIG 3). Right parathyroid adenoma posterior to the middle third of the thyroid lobe: right superior parathyroid adenoma in location 1. EPLA is indicated.
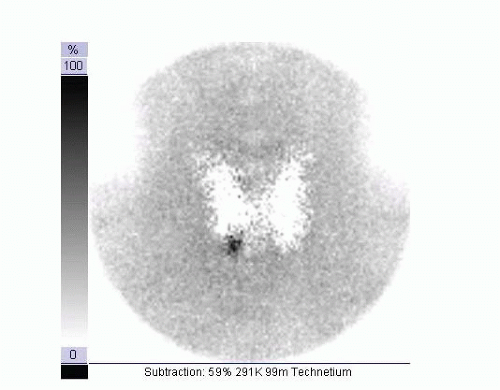
FIG 5 • Parathyroid Tc-99m sestamibi scintigraphy; subtraction protocol. The subtraction image demonstrates a right parathyroid adenoma at the level of the inferior third of the right thyroid lobe.
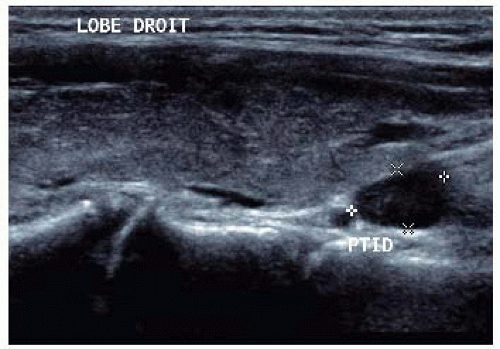
FIG 6 • Ultrasound (same patient in FIG 5). Right parathyroid adenoma posterior to the inferior third of the thyroid lobe: right, more probably inferior, parathyroid adenoma in location 2. EPLA is indicated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access