2E01
Key word: Diagnosis of Division of Intercostobrachial Nerve
Author: Vicente Valero III, MD
Editor: Bradford D. Winters, MD, PhD
A 62-year-old woman presents to your clinic after undergoing a left modified radical mastectomy for stage III breast carcinoma. She has done well postoperatively and is concerned only about new onset numbness and tingling over the posteromedial aspect of her left upper arm. She has normal strength, no motor deficits, and normal range of motion in her left upper extremity. What structure was likely injured during her operation?

Intercostobrachial nerve

Long thoracic nerve of Bell

Medial cutaneous nerve of arm

Medial pectoral nerve

Thoracodorsal nerve
View Answer
Answer: (A) Intercostobrachial nerve
Rationale:
The intercostobrachial nerve is a lateral cutaneous branch of the second intercostal nerve arising from T2. It supplies sensation for the posteromedial portion of the upper arm. This nerve is at risk of injury during the axillary lymph node dissection (ALND) portion of a modified radical mastectomy. The course of the intercostobrachial nerve can be traced as it penetrates through the intercostal muscles and the serratus anterior in the midaxillary line. It subsequently traverses the axilla where the posterior branch provides sensation to the posterior axillary fold and then travels into the upper arm. It is important to preserve this nerve during ALND in order to prevent postoperative paresthesias and sensory deficits in the ipsilateral upper arm. A small prospective study demonstrated that preservation of the intercostobrachial nerve increases operative time by a median time of 5 minutes. Due to the variable anatomy associated with the intercostobrachial nerve and the overall sensory supply to the axilla and the upper arm, sensory abnormalities following ALND can still occur despite preservation of the intercostobrachial nerve. It should also be noted that this nerve might need to be sacrificed in some patients in order to achieve a satisfactory oncologic specimen with adequate nodal tissue.
References:
Abdullah TI, Iddon J, Barr L, et al. Prospective randomized controlled trial of preservation of the intercostobrachial nerve during axillary node clearance for breast cancer. Br J Surg. 1998;85(10):1443-1445.
Freeman SR, Washington SJ, Pritchard T, et al. Long term results of a randomised prospective study of preservation of the intercostobrachial nerve. Eur J Surg Oncol. 2003;29(3):213-215.
Loukas M, Hullett J, Louis RG Jr, et al. The gross anatomy of the extrathoracic course of the intercostobrachial nerve. Clin Anat. 2006;19(2):106-111.
2E02
Key word: Diagnosis of Intraoperative Nerve Injury
Author: Seth D. Goldstein, MD
Editor: Bradford D. Winters, MD, PhD
A 58-year-old woman with biopsy-proven papillary thyroid carcinoma and clinically involved right cervical lymph nodes undergoes total thyroidectomy and right modified radical neck dissection. On the first morning postoperatively, a focused clinical examination should include an assessment of which of the following?

Grip strength

Hand sensation

Plantar flexion

Shoulder shrug

Tongue protrusion
View Answer
Answer: (D) Shoulder shrug
Rationale:
Radical neck dissection is the en bloc removal of all nodal groups with surrounding structures between the mandible and the clavicle. Modified radical neck dissection attempts the same node removal while sparing the sternocleidomastoid muscle, the internal jugular vein, and the spinal accessory nerve (cranial nerve XI). The spinal accessory nerve runs through the operative field and is at risk for injury. Its function can be assessed by examining the range of motion and strength of the ipsilateral sternocleidomastoid and trapezius muscles. Intraoperative nerve injury affecting grip strength and hand sensation (brachial plexus), tongue protrusion (hypoglossal nerve, cranial nerve XII), or plantar flexion (tibial nerve via sciatic) would not be expected.
Reference:
Mandpe AH. Neck neoplasms and neck dissection. In: Lalwani AK, ed. Current Diagnosis & Treatment in Otolaryngology-Head & Neck Surgery. 3rd ed. New York, NY: McGraw-Hill; 2012.
2E03
Key word: Diagnostic Test for Recurrence of ITP
Author: Seth D. Goldstein, MD
Editor: F. Dylan Stewart, MD, FACS
A 15-year-old boy presents 1 year following laparoscopic splenectomy for idiopathic thrombocytopenic purpura (ITP). He reports spontaneous massive epistaxis and is found to have a platelet count of 10,000/µL. In addition to a complete blood count, which of the following is the most helpful initial study to send based on his past history?

Bone marrow aspirate

Partial thromboplastin time

Peripheral blood smear for eosinophils

Peripheral blood smear for Howell-Jolly bodies

Prothrombin time
View Answer
Answer: (D) Peripheral blood smear for Howell-Jolly bodies
Rationale:
Idiopathic (or immune) thrombocytopenic purpura (ITP) can be acute or chronic. Acute ITP occurs mostly in children; often follows a viral infection; has an excellent prognosis, with most cases resolving spontaneously without treatment; and is the most common type of ITP. Chronic ITP occurs mostly in adults, affects women more often than men, and only rarely resolves spontaneously.
Splenectomy is indicated for ITP refractory to medical management, usually corticosteroids and intravenous immunoglobulin (IVIG), and is efficacious in almost two-thirds of patients. A laparoscopic approach may result in a faster hospital recovery, but controversy exists regarding whether open surgery may more effectively allow for scrutiny of an accessory spleen. Howell-Jolly bodies are histologic findings of asplenia on peripheral blood smear. If Howell-Jolly bodies appeared initially after surgery but are no longer present, an accessory spleen is suspected. Resection of an accessory spleen for recurrent ITP is still controversial due to a lack of strong evidence for its efficacy. Bone marrow aspirate can be checked to rule out an inappropriate initial diagnosis, but peripheral blood smear would still be the first laboratory test performed. A complete history again to look for possible drug-related thrombocytopenia or a new diagnosis of HCV or HIV is also indicated.
Reference:
Fraker DL. Spleen. In: Doherty GM, ed. Current Diagnosis & Treatment: Surgery. 13th ed. Columbus, OH: The McGraw-Hill Companies, Inc; 2010.
2E04
Key word: Diagnostic Test for a Tender Breast Mass
Author: Seth D. Goldstein, MD
Editor: Lisa K. Jacobs, MD
A 25-year-old woman presents with a breast mass found on self-examination. A 3-cm tender mass is palpable in the upper outer quadrant of the right breast with no overlying skin changes. The patient has no medical history and takes only an oral contraceptive pill. What is the most appropriate initial imaging modality?

Computed tomography (CT)

Magnetic resonance imaging (MRI)

Mammogram

Positron emission tomography (PET)

Ultrasound
View Answer
Answer: (E) Ultrasound
Rationale:
Assessment of a breast mass should include clinical examination, imaging, and biopsy. In women under 30, ultrasound is the recommended initial imaging modality. Ultrasound can differentiate between solid and cystic masses and can also guide fine-needle aspiration. In this younger age group, mammography is less useful even with the use of digital subtraction technology due to the higher breast density. MRI is highly sensitive but is not used for screening, while PET would only be used for suspicion of metastatic disease.
Reference:
Laronga C, Tollin S, Turaga KK. History, physical examination, and staging. In: Kuerer HM, ed. Kuerer’s Breast Surgical Oncology. New York, NY: McGraw-Hill; 2010.
2E05
Key word: Findings of Acute Adrenal Insufficiency
Author: Kelly Olino, MD
Editor: Bradford D. Winters, MD, PhD
An otherwise healthy 52-year-old male is in the postoperative care unit hours after undergoing an uncomplicated left-sided laparoscopic adrenalectomy for a 0.5-cm cortisol-producing tumor when he is noted to have a heart rate of 82 beats per minute and blood pressure of 90/40 mm Hg. After administering 2 L of normal saline, the blood pressure is unchanged. The most critical next step in management will be to:

Administer 100-mg IV hydrocortisone

Begin a norepinephrine drip

Check troponin levels

Obtain a 12-lead EKG

Obtain a portable chest x-ray
View Answer
Answer: (A) Administer 100-mg IV hydrocortisone
Rationale:
Hypotension following abdominal surgery is a common complication encountered in the recovery room. A cortisol-producing tumor leads to suppression of the hypophyseal-pituitary-adrenal axis, and the contralateral adrenal gland is usually atrophied and poorly functional as a result. Suppression of the hypophyseal-pituitary-adrenal axis may last up to a year after surgery. Following the resection of a cortisol-producing tumor, perioperative corticosteroids are therefore required, followed by corticosteroid replacement for several weeks after surgery. In this example, all of the other choices are viable options and should be part of the differential workup, but if steroids are not administered, the hypotension from acute adrenal insufficiency will not resolve.
Reference:
Gauger PG. Complications of adrenal surgery. In: Mulholland MW, Doherty GM, eds. Complications in Surgery. Philadelphia, PA: Lippincott, Williams & Wilkins; 2006:535-549.
2E06
Key word: Findings in Vitamin D Deficiency
Author: Kelly Olino, MD
Editor: Elizabeth C. Wick, MD
A 55-year-old postmenopausal woman is found to have osteoporosis and joint and muscle aches 1 year following roux-en-Y gastric bypass surgery and a 68 kg (150 lb) weight loss from her preoperative weight of 163 kg (360 lb). During workup for her condition she is noted to have a calcium level of 7.8 mg/dL. Further laboratory analysis will likely show the following:

PTH = 20 pg/mL, Vitamin D = 15 ng/mL, Phosphate = 3.5 mg/dL

PTH = 25 pg/mL, Vitamin D = 20 ng/mL, Phosphate = 3.5 mg/dL

PTH = 100 pg/mL, Vitamin D = 15 ng/mL, Phosphate = 3.5 mg/dL

PTH = 100 pg/mL, Vitamin D = 15 ng/mL, Phosphate = 6 mg/dL

PTH = 100 pg/mL, Vitamin D = 30 ng/mL, Phosphate = 3.5 mg/dL
View Answer
Answer: (C) PTH = 100 pg/mL, Vitamin D = 15 ng/mL, Phosphate = 3.5 mg/dL
Rationale:
The patient has secondary hyperparathyroidism due to vitamin D deficiency. The gastric bypass procedure leads to a lack of vitamin D absorption through both the functional partial gastrectomy and the malabsorption caused by the roux limb bypass. With vitamin D deficiency, the calcium level is usually normal, the PTH level is elevated, both vitamin D and 25-OH Vitamin D levels are low, and the phosphate level is normal. Only choice (C), therefore, has laboratory findings consistent with secondary hyperparathyroidism. Vitamin D deficiency is usually asymptomatic but can also manifest in children in the form of rickets or in elderly patients in the form of osteomalacia with concomitant muscle and bony aches.
Reference:
Johnson JM, Maher JW, DeMaria EJ, et al. The long-term effects of gastric bypass on vitamin D metabolism. Ann Surg. 2006;243(5):701-704.
2E07
Key word: Indications for Excisional Biopsy of Breast Mass
Author: Seth D. Goldstein, MD
Editor: Lisa K. Jacobs, MD
A 47-year-old woman presents with a palpable breast mass discovered on self-examination. Mammography demonstrates a Breast Imaging-Reporting and Data System (BI-RADS) 4 lesion found to be a 2-cm spiculated mass with heterogeneous calcifications. Core-needle biopsy is read as atypia without malignant features. The best next step would be the following:

Excisional biopsy

Incisional biopsy

Mastectomy

Repeat needle biopsy

Surveillance with yearly mammography
View Answer
Answer: (A) Excisional biopsy
Rationale:
Needle biopsy is generally sufficient to guide surgical management of a breast mass. Exceptions are tumors that cannot be biopsied (e.g., subareolar, posterior position in a large breast) and when discordance exists between biopsy results and other clinical findings. Lesions with a high level of radiologic suspicion (BI-RADS 4 or 5) are usually evaluated first by using a core-needle biopsy, which is typically diagnostic. However, in this case, benign findings from the biopsy do not match well with the level of radiologic suspicion (BI-RADS 4), which indicates a high likelihood of malignancy. Given this degree of discordance, the biopsy may represent a false negative due to sampling error, necessitating the use of excisional biopsy for ultimate diagnosis.
References:
King TA, Morrow M. Breast disease. In: Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery: Scientific Principles and Practice. 5th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2011.
Montgomery L. Excisional breast biopsy. In: Kuerer HM, ed. Kuerer’s Breast Surgical Oncology. New York, NY: McGraw-Hill; 2010.
2E08
Key word: Initial Treatment of Adrenal Mass
Author: Kelly Olino, MD
Editor: Richard D. Schulick, MD, MBA, FACS
A 56-year-old woman is found to have a 2-cm mass in her left adrenal gland following an abdominal computed tomography (CT) scan performed following a motor vehicle collision. Which of the following is the best next step in management of this adrenal mass?

Laparoscopic adrenalectomy

Mammography

Measurement of adrenocorticotropic hormone (ACTH) level, 24-hour urine-free cortisol level, urine metanephrine level, and calculate an aldosterone/renin ratio

Metaiodobenzylguanidine (MIBG) scan

Observation with repeat abdominal CT scan in 1 year
View Answer
Answer: (C) Measurement of adrenocorticotropic hormone (ACTH) level, 24-hour urine-free cortisol level, urine metanephrine level, and calculate an aldosterone/renin ratio
Rationale:
An adrenal incidentaloma is a lesion greater than 1 cm found by coincidence on a radiographic study done for other reasons. The prevalence of incidentalomas ranges from 1% to 10% and rises with increasing age. The differential diagnosis of an adrenal incidentaloma includes aldosteronoma, pheochromocytoma, cortisol-producing tumor, sex hormone-secreting tumor, metastasis, nonfunctional adenoma/myelolipoma, and adrenocortical carcinoma.
The first step in management is to perform a thorough history and physical examination looking for hypertension or a change in the number of blood pressure medications, hirsutism, weight changes, headaches, flushing, palpitations, or a personal or family history of malignancy or genetic syndromes. Laboratory evaluation is also necessary to rule out the presence of a functional cortisol-secreting mass, and is performed by measuring an ACTH level and a 24-hour urine-free cortisol level or performing a 1-mg overnight dexamethasone suppression test with a morning cortisol level drawn. A pheochromocytoma workup should include urine or plasma metanephrines and normetanephrines. Aldosteronoma workup consists of measuring serum potassium and the serum aldosterone/renin ratio. Sex hormone-secreting tumors are rare, but testosterone or dehydroepiandrosterone (DHEA) levels can be measured if clinical symptoms are present.
Radiographic imaging with triple phase CT imaging or MRI is a useful adjunct as well. Nonfunctional adrenocortical adenomas on triple phase CT scan will measure <10 Hounsfield units (HU) on dry scan and have >50% washout after 10 minutes on delayed phase. Adrenocortical carcinomas are usually >4 cm, irregular, hypervascular, and >10 HU and have <50% washout; they can also have hemorrhage, calcification, or necrosis. Pheochromocytomas are regular, hypervascular, and >10 HU and have <50% washout. They are characteristically hyperintense on T2-weighted MRI. Aldosteronomas are usually smaller masses, and careful attention has to be made to ensure that bilateral adrenal hyperplasia is not present. Metastases can be bilateral, and radiographic findings associated with primary cancers (especially lung, breast, stomach, kidney, melanoma, and lymphoma) should be sought. Indications for adrenalectomy include a functional adrenal mass, size >4 cm or other features indicative of adrenocortical carcinoma, and an interval increase in size >1 cm.
Reference:
Zeiger MA, Thompson GB, Duh QY, et al. American Association of Clinical Endocrinologists and American Association of Endocrine Surgeons Medical Guidelines for the Management of Adrenal Incidentalomas: executive summary of recommendations. Endocr Pract. 2009;15(5):450-453.
2E09
Key word: Most Common Nerve Injured during Total Thyroidectomy
Author: Jacqueline Garonzik-Wang, MD, PhD
Editor: Alan P.B. Dackiw, MD, PhD, BSc, BSc(Med), FACS, FRCSC
After an uneventful total thyroidectomy, a 58-year-old female is found to have a weak voice and difficulty coughing in the recovery room. She is hemodynamically stable with 95% saturation on 2 L oxygen via nasal canal. Her examination is unremarkable, and her wound is intact without drainage or evidence of a hematoma. Direct laryngoscopy is performed at the bedside, and her right vocal cord is noted to be in a fixed position. What is the most likely cause of her symptoms?

Complete transection of the right recurrent laryngeal nerve (RLN)

Compression from a submuscular bleed and hematoma

Stretch injury to the right RLN

Transection of the external branch of the superior laryngeal nerve (EBSLN)

Trauma secondary to endotracheal intubation
View Answer
Answer: (C) Stretch injury to the right RLN
Rationale:
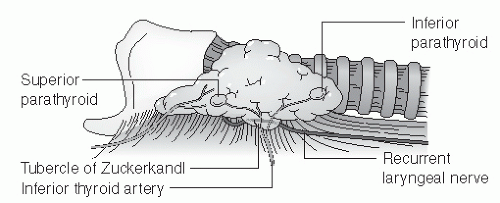
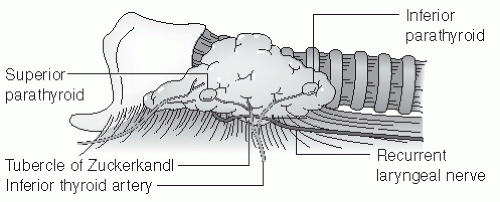
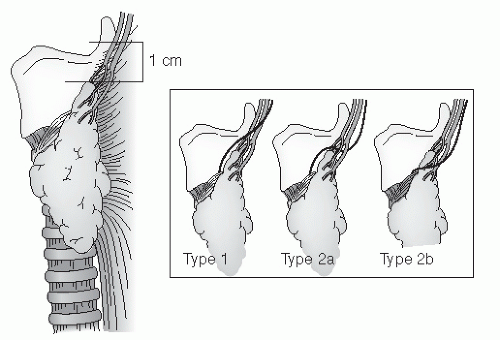
Total thyroidectomy has become the preferred treatment for thyroid cancer, especially for lesions larger than 1 cm. Nerve injuries, while infrequent, can lead to significant morbidity, and therefore, appropriate preoperative counseling is warranted. RLN injury is the most common nerve injury identified after total thyroidectomy. Unilateral RLN injury often results in hoarseness and a weak cough. The RLN innervates all intrinsic muscles of the larynx and vocal cords (except the cricothyroid muscle), and therefore, it is not surprising that injury results in altered phonation. Furthermore, on direct visualization, the ipsilateral vocal cord is fixed and can be found in an abducted or paramedian position. Bilateral RLN injury, a possible complication of total thyroidectomy, can result in airway obstruction requiring a tracheostomy.
The EBSLN innervates the cricothyroid muscle. Injury to this nerve results in difficulty with voice projection and fatigue at higher pitches. While endotracheal tube trauma can cause hoarseness, the findings on direct laryngoscopy make RLN injury the correct answer. In addition, given the lack of physical examination findings, a neck hematoma is also unlikely. Finally, while RLN transection always results in ipsilateral cord paralysis, transection is less likely following direct visualization making other forms of temporary neuropraxia more likely, such as stretch injury. If complete transection occurs and is noticed intraoperatively, surgical repair at the time of surgery should be attempted.
References:
Chiang FY, Wang LF, Huang YF, et al. Recurrent laryngeal nerve palsy after thyroidectomy with routine identification of the recurrent laryngeal nerve. Surgery. 2005;137:342-347.
Goncalves Filho J, Kowalski LP. Surgical complications after thyroid surgery performed in a cancer hospital. Otolaryngol Head Neck Surg. 2005;132:490-494.
Netterville JL, Aly A, Ossoff RH. Evaluation and treatment of complications of thyroid and parathyroid surgery. Otolaryngol Clin North Am. 1990;23:529-552.
2E10
Key word: Operative Approach to Splenectomy
Author: Jacqueline Garonzik-Wang, MD, PhD
Editor: Mark D. Duncan, MD, FACS
In which of the following patients is laparoscopic splenectomy contraindicated and an open approach required?

18-year-old with hereditary spherocytosis and splenomegaly (spleen greater than 20 cm in length)

36-year-old morbidly obese female with a body mass index (BMI) of 38 kg/m
2
52-year-old male with cirrhosis and portal hypertension

61-year-old female with idiopathic thrombocytopenic purpura and a platelet count of 45,000/mm
3
68-year-old male with a splenic lymphangiosarcoma
View Answer
Answer: (C) 52-year-old male with cirrhosis and portal hypertension
Rationale:
Laparoscopic splenectomy has become the standard and recommended approach for almost all benign and malignant disorders requiring elective splenectomy. A laparoscopic approach has been shown to decrease operative times, postoperative length of stay, and postoperative complications. This holds true regardless of body habitus and age. In addition, a laparoscopic approach is even recommended for patients with splenomegaly. While splenomegaly used to be considered a relative contraindication to a laparoscopic approach, more recent reports have demonstrated that laparoscopic splenectomy is feasible and safe in the hands of an experienced laparoscopic surgeon and can be attempted regardless of size. Patients with massive splenomegaly might benefit from a “hand-assisted” laparoscopic approach. Splenomegaly does, however, increase the risk of conversion to an open procedure.
While there have been some reports showing that laparoscopic splenectomy can be performed safely in patients with liver disease and cirrhosis, experts in this field still consider portal hypertension secondary to cirrhosis to be a contraindication to the laparoscopic approach. For these patients, the risk of intraoperative hemorrhage is too high. For patients with thrombocytopenia or coagulopathy, attempts should be made to correct their platelet counts and/or coagulopathy prior to surgery (or at the time of surgery in the case of thrombocytopenia), but a laparoscopic approach is still feasible.
Reference:
Habermalz B, Sauerland S, Decker G, et al. Laparoscopic splenectomy: the clinical practice guidelines of the European Association for Endoscopic Surgery (EAES). Surg Endosc. 2008;22(4):821-848.
2E11
Key word: Pathologic Diagnosis of High-risk Breast Cancer
Author: Jacqueline Garonzik-Wang, MD, PhD
Editor: Lisa K. Jacobs, MD
A 53-year-old woman was found to have a suspicious lesion on routine screening mammography. She subsequently underwent stereotactic core biopsy of the lesion. Which of the following pathologic findings puts her at greatest risk of breast cancer?
 Measurement of adrenocorticotropic hormone (ACTH) level, 24-hour urine-free cortisol level, urine metanephrine level, and calculate an aldosterone/renin ratio
Measurement of adrenocorticotropic hormone (ACTH) level, 24-hour urine-free cortisol level, urine metanephrine level, and calculate an aldosterone/renin ratio