Endocrine, Hematic, Lymphatic, and Breast
1E01
Key word: Treatment of Metastatic VIPoma
Author: Justin B. Maxhimer, MD
Editor: Anne O. Lidor, MD, MPH
A 39-year-old female presents to the emergency department with complaints of watery diarrhea and upper abdominal pain for the past 2 weeks. On workup, she is found to have a small mass in the body of the pancreas on computed tomography scanning. Laboratory abnormalities include a hemoglobin of 8.7 mg/dL, white blood cell count of 10.1, hypokalemia, and a metabolic acidosis. She is subsequently scheduled to have an exploratory laparotomy. Intraoperatively, the mass is removed from her pancreas and multiple small nodules are found in her liver. Considering the most likely diagnosis, what are her best treatment options?
View Answer
Answer: (A) 5-fluorouracil and interferon-alpha
Rationale:
In 1958, Verner and Morrison described a syndrome of watery diarrhea, hypokalemia, and achlorhydria (WDHA). These have subsequently been named VIPomas, after the excess of the hormone Vasoactive Intenstinal Peptide. VIPomas in adults are usually neuroendocrine islet cell tumors of the pancreas that produce high amounts of VIP. Other secreted hormones may include secreted gastrin and pancreatic polypeptide. Clinical diagnosis is based on a history of approximately 10 watery stools per day. Fecal losses while fasting are at least 20 mL/kg/day but exceed 50 mL/kg/day in most cases. Fecal loss of large amounts of potassium and bicarbonate cause hypokalemia, acidosis, and volume depletion.
Surgical exploration with tumor resection leads to cure in 50% of patients. In patients with metastatic disease, there are a number of treatment options. In advanced stages of the disease, tumor debulking may relieve symptoms but is not effective in all cases. In adults, selected patients have had orthotopic liver transplantation. Serum VIP levels may normalize within an hour after curative tumor resection. Repetitive embolization of the hepatic artery may provide palliation over a long period for patients with liver metastases but is not curative. Somatostatin analogs and conventional chemotherapy regimens have been effective in controlling some of the symptoms but were not effective on VIPoma syndrome and tumor progression. The combination of 5-fluorouracil and interferon-alpha has been found to result in major clinical improvement associated with tumor regression.
References:
Doherty GM. Rare endocrine tumours of the GI tract. Best Pract Res Clin Gastroenterol. 2005;19:807-817.
Marks IN, Bank S, Louw JH. Islet cell tumor of the pancreas with reversible watery diarrhea and achylorhydria. Gastroenterology. 1967;52(4):695-708.
1E02
Key word: Characteristics of Solid and Cystic Cancer of the Thyroid
Author: Robert A. Meguid, MD, MPH
Editors: Martha A. Zeiger, MD, FACS, and Konstantinos I. Makris, MD
A 52-year-old woman presents to your clinic with a palpable thyroid nodule. Ultrasound shows a 3-cm lesion in the right thyroid lobe with solid and cystic components. Ultrasound-guided fine-needle aspiration (FNA) reveals a thyroid cancer. Which of the following is the most likely diagnosis?
View Answer
Answer: (D) Papillary carcinoma
Rationale:
Thyroid cancer may be divided histologically into (1) well-differentiated (papillary, follicular variant of papillary, follicular, and Hürthle cell) carcinoma, (2) medullary carcinoma, and (3) undifferentiated or anaplastic carcinoma.
Papillary carcinoma constitutes 80% of all thyroid cancers. On histology, the tumor cells have the characteristic “Orphan Annie eye” (empty-appearing nuclei) appearance, and psammoma bodies are typically present. Papillary carcinoma is multifocal at presentation 75% of the time. Therefore, treatment of lesions 1 cm or larger consists of total thyroidectomy. Central (level VI) neck lymph node dissection is added if suspicious nodes are present or the estimated risk of recurrence is high (prophylactic central neck dissection is advocated by many endocrine surgeons as well). Patients are usually treated with 131I postoperatively based on their estimated risk of recurrence. Papillary carcinoma is associated with a 90% 10-year survival.
Follicular carcinoma constitutes approximately 15% of well-differentiated thyroid cancers. FNA results may be suggestive of a follicular neoplasm, but a diagnosis of cancer can only be made on final histopathology with documentation of vascular or capsular invasion. Treatment is total thyroidectomy followed by postoperative 131I. Ten-year survival is estimated at 85%.
Medullary carcinoma constitutes less than 1% of all thyroid cancers, and arises from the neuroendocrine parafollicular C cells. Fifteen percent of cases are associated with MEN 2A and IIb syndromes. FNA is diagnostic with positive immunostaining for calcitonin. Medullary carcinoma should be treated with total thyroidectomy and central neck dissection at a minimum. Modified radical neck dissection is indicated for lateral cervical lymphadenopathy. The overall 10-year survival is 50%.
References:
Cooper DS, Doherty GM, Haugen BR, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19(11):1167-1214.
Suliburk J, Delbridge L. Surgical management of well-differentiated thyroid cancer: State of the art. Surg Clin North Am. 2009;89(5):1171-1191.
1E03
Key word: Conditions Associated with Tertiary Hyperparathyroidism
Author: Robert A. Meguid, MD, MPH
Editors: Martha A. Zeiger, MD, FACS, and Konstantinos I. Makris, MD
A 55-year-old woman presents to your clinic with the new diagnosis of tertiary hyperparathyroidism. Which of the following operations has she most likely previously undergone?
View Answer
Answer: (C) Renal transplantation
Rationale:
Tertiary hyperparathyroidism is persistent abnormal hypersecretion of parathyroid hormone (PTH) after correction of causes of secondary hyperparathyroidism. Primary hyperparathyroidism is due to inappropriate secretion of PTH caused by a parathyroid adenoma or parathyroid hyperplasia. Secondary hyperparathyroidism is a result of compensatory increase of PTH secretion in response to hypocalcemia from nonparathyroid cause. This is most commonly due to renal failure, which causes hyperphosphatemia, hypovitaminosis D, and resultant hypocalcemia.
Classically, tertiary hyperparathyroidism is seen in the setting of a patient with long-standing secondary hyperparathyroidism, who has had a renal transplant for dialysis-dependent renal failure. The compensatory hypersecretion of PTH of secondary hyperparathyroidism persists after correction of the renal failure and becomes autonomous (tertiary hyperparathyroidism) as a result of parathyroid hyperplasia or new parathyroid adenoma. Patients usually present with normal to high calcium levels, and elevated PTH levels.
Indications for surgery in tertiary hyperparathyroidism include severe hypercalcemia (>11.5 mg/dL), persistent hypercalcemia (>10.2 mg/dL) for more than 3 months to 1 year after renal transplant, and severe osteopenia and persistent symptoms of hyperparathyroidism (bone and joint pain, pathologic fractures, generalized muscular weakness, fatigue, renal stones, mental status changes, peptic ulcer disease, pancreatitis, and calciphylaxis).
Surgical management is either subtotal (three and a half glands) parathyroidectomy or total parathyroidectomy with autotransplantation.
References:
Guerrero MA, Rahbari R, Kebebew E. Secondary and tertiary hyperparathyroidism. In: Cameron JL, Cameron AM eds. Current Surgical Therapy. 10th ed. Philadelphia, PA: Mosby; 2011:617-620.
Irvin GL 3rd, Solorzano CC, Carneiro DM. Quick intraoperative parathyroid hormone assay: Surgical adjunct to allow limited parathyroidectomy, improve success rate, and predict outcome. World J Surg. 2004;28(12):1287-1292.
Pitt SC, Sippel RS, Chen H. Secondary and tertiary hyperparathyroidism, state of the art surgical management. Surg Clin North Am. 2009;89(5):1227-1239.
1E04
Key word: Treatment of Phyllodes Tumor of the Breast
Author: Nikiforos Ballian, MBBS
Editors: Theodore N. Tsangaris, MD, and Mehran Habibi, MD, MBA
A 47-year-old woman presents with a rapidly enlarging 5-cm right breast mass without palpable axillary nodes. Fine-needle aspiration (FNA) is nondiagnostic. Core biopsy is performed and results are reported as equivocal, but suggestive of a phyllodes neoplasm. The appropriate next step in management is:
View Answer
Answer: (D) Tumor excision with a 1-cm margin
Rationale:
Phyllodes tumors are breast neoplasms composed of an epithelial component, which is always benign, and a stromal component that can be benign (60%), borderline (15%), or frankly malignant (25%). They account for less than 1% of all breast tumors and share morphologic similarities with fibroadenomas, but their peak incidence is in the fourth and fifth decades of life. Phyllodes neoplasms present as breast masses, sometimes rapidly enlarging, but rarely cause additional symptoms. Mammography and ultrasound cannot reliably distinguish fibroadenoma from phyllodes tumor, while fine-needle aspiration is diagnostic only in a minority of cases. Core-needle biopsy is more accurate, although recent studies have failed to yield consistent recommendations regarding its use.
Due to rapid growth and potential for malignancy, surgical treatment of phyllodes tumors is mandatory. Simple tumor enucleation is insufficient due to high recurrence rates, even for benign tumors. There is no role for sentinel node biopsy because malignant phyllodes tumors behave like sarcomas, rarely causing lymph node metastases. Recent data suggest that wide local excision with a 1-cm margin is adequate even for malignant tumors, yielding the same survival despite higher local recurrence rates.
References:
Ben Hassouna J, Damak T, Gamoudi A, et al. Phyllodes tumors of the breast: A case series of 106 patients. Am J Surg. 2006;192:141-147.
Chen WH, Cheng SP, Tzen CY, et al. Surgical treatment of phyllodes tumors of the breast: Retrospective review of 172 cases. J Surg Oncol. 2005;91:185-194.
Foxcroft LM, Evans EB, Porter AJ. Difficulties in the preoperative diagnosis of phyllodes tumours of the breast: A study of 84 cases. Breast. 2007;16:27-37.
Iglehart JD, Kaelin CM. Diseases of the breast. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 17th ed. Philadelphia, PA: Elsevier; 2004:867-928.
Macdonald OK, Lee CM, Tward JD, et al. Malignant phyllodes tumor of the female breast: Association of primary therapy with cause-specific survival from the Surveillance, epidemiology, and end results (SEER) program. Cancer. 2006;107:2127-2133.
1E05
Key word: Etiology of Cushing Syndrome
Author: Robert A. Meguid, MD, MPH
Editor: Alan P.B. Dackiw, MD, PhD, BSc, BSc(Med), FACS, FRCSC
A 38-year-old woman is referred to your clinic after an elevated 24-hour urine Cortisol measurement. She is not on any steroids. What is the most likely cause of this patient’s disease?
View Answer
Answer: (E) Pituitary adenoma
Rationale:
Cushing syndrome is the condition resulting from excessive glucocorticoid exposure. Causes can be divided into iatrogenic or noniatrogenic, and adrenocorticotropic hormone (ACTH)-dependent or ACTH-independent categories.
Iatrogenic Cushing syndrome is due to high-dose exogenous glucocorticoid administration, usually for treatment of nonendocrine disorders.
ACTH-dependent causes include ACTH-secreting pituitary adenoma and ectopic ACTH syndrome. ACTH-secreting pituitary adenoma, or Cushing disease, constitutes 68% of noniatrogenic Cushing syndrome. Most patients are female and 20 to 40 years of age. The disease progresses slowly, and clinical features include hirsutism and acne. Ectopic ACTH syndrome constitutes 15% of noniatrogenic Cushing syndrome. Most patients are female and of 40 to 60 years of age. ACTH is usually secreted by small-cell carcinomas of the lung, and bronchial carcinoid tumors, but may also be secreted by other carcinoid tumors, pheochromocytomas, pancreatic islet cell tumors, medullary thyroid, and ovarian cancers. The disease progresses rapidly, associated with the primary cancer, and clinical features include hypertension, weakness and hypokalemia, glucose intolerance, and hyperpigmentation.
ACTH-independent causes include functioning adrenocorticoid tumors, with adrenal adenomas accounting for 9% of noniatrogenic Cushing syndrome, and adrenal carcinomas for 8%. Most patients are female and of 35 to 40 years of age. In the case of adrenal adenomas secreting cortisol, onset is usually gradual. For adrenal carcinomas, onset is rapid.
Diagnosis is made via a 24-hour urine cortisol measurement or a dexamethasone suppression test. Localization is via CT or MRI; however, due to the microadenomatous nature of most pituitary adenomas, frequently none are seen on imaging.
Reference:
McPhee SJ. Disorders of the hypothalamus and pituitary gland. In: McPhee SJ, Lingappa VR, Ganong WF, Lange JD, eds. Pathophysiology of Disease. 3rd ed. New York, NY: Lange Medical Books/McGraw-Hill; 2000:509-517.
1E06
Key word: Treatment of Lobular Carcinoma In Situ of the Breast
Author: Jacqueline Garonzik-Wang, MD, PhD
Editors: Julie R. Lange, MD, ScM, FACS, and Mehran Habibi, MD, MBA
A 40-year-old premenopausal woman is seen by her physician for evaluation of a breast nodule. Physical examination confirms the presence of a 1-cm movable mass; mammogram and ultrasound evaluation are both found to be consistent with a fibroadenoma. A core biopsy confirms this diagnosis. The lesion is excised at the patient’s request. Pathology results reveal a fibroadenoma with a small area of lobular carcinoma in situ (LCIS) in the surrounding breast tissue, focally extending to one margin. The next step in management is:
View Answer
Answer: (B) Counsel the patient about their future breast cancer risk and screening options
Rationale:
LCIS can be found incidentally on biopsy performed for other reasons. This finding, sometimes referred to as lobular neoplasia, is considered to be a marker of increased risk of subsequent breast cancer development. The implied risk extends over all breast tissue, bilaterally. Women should receive counseling about their increased risk of breast cancer, which can be approximately 25% over their lifetime. The simplest management option is careful screening with annual mammography and clinical examination. Some women may consider chemoprevention with a 5-year course of tamoxifen, which is expected to lower the risk of invasive breast cancer by about half. Postmenopausal women, particularly those with osteoporosis, may consider raloxifene for similar risk reduction. Bilateral prophylactic mastectomy is a more aggressive risk-reduction measure and is sometimes considered by women who have breasts that are difficult to screen or those with high levels of anxiety, or in women with other strong risk factors such as known deleterious BRCA mutation or a strong family history of breast cancer.
References:
McAuliffe PF, Andtbacka RHI, Robinson EK, et al. Noninvasive breast cancer. In: Feig BW, Ching CD, eds. The M.D. Anderson Surgical Oncology Handbook. 5th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2012.
Wang TN, Bland KI. Ductal and lobular carcinoma in situ of the breast. In: Cameron JL, Cameron AM, eds. Current Surgical Therapy. 10th ed. Philadelphia, PA: Mosby; 2011:542-546.
1E07
Key word: Increased Cancer Incidence with Tamoxifen Therapy
Author: Jonathan A. Forbes, MD
Editors: Julie R. Lange, MD, ScM, FACS, and Mehran Habibi, MD, MBA
A 64-year-old postmenopausal woman with Estrogen Receptor Positive (ER+), stage I breast cancer presents following lumpectomy, and radiation therapy, now on therapy with tamoxifen. She asks about the risks of tamoxifen therapy. You tell her that:
 Tamoxifen has been linked to an increased risk of developing endometrial adenocarcinoma and uterine sarcoma
Tamoxifen has been linked to an increased risk of developing endometrial adenocarcinoma and uterine sarcoma Tamoxifen increases bone resorption, increasing risk of long bone and pelvic fractures due to osteoporosis
Tamoxifen increases bone resorption, increasing risk of long bone and pelvic fractures due to osteoporosisView Answer
Answer: (B) Tamoxifen has been linked to an increased risk of developing endometrial adenocarcinoma and uterine sarcoma
Rationale:
Tamoxifen is a selective estrogen receptor modulator (SERM) that acts as an estrogen agonist in certain organs of the body (uterus, bone) and an estrogen antagonist in others (breast). The most commonly recognized serious risks of tamoxifen therapy include development of deep venous thrombosis (DVT) and resulting pulmonary emboli, and development of endometrial hyperplasia and endometrial cancer. The risks of venous thrombosis and endometrial cancer in women on tamoxifen therapy are higher in postmenopausal women than in premenopausal women. Other, less threatening risks associated with tamoxifen therapy include hot flashes and mood changes.
Postmenopausal women who take tamoxifen are approximately two to three times more likely than those not taking tamoxifen to develop endometrial cancer. This risk appears to increase with duration of tamoxifen therapy. The Surveillance Epidemiology and End Results (SEER) database of the National Cancer Institute has recently shown that tamoxifen exposure increases the risk of uterine sarcomas (especially malignant mixed müllerian tumors [MMMT]), in addition to endometrial adenocarcinomas. Because the risks of tamoxifen therapy increases with time and the benefits of tamoxifen therapy beyond 5 years have not yet been demonstrated, the American College of Obstetricians and Gynecologists currently recommends to limit tamoxifen use to no longer than 5 years. Tamoxifen use is associated with lower risk of developing a primary breast cancer in the contralateral breast and
in some circumstances can be offered to women at high risk of breast cancer as a risk-reduction measure.
in some circumstances can be offered to women at high risk of breast cancer as a risk-reduction measure.
Tamoxifen provides some protection against postmenopausal bone loss. However, the increase in bone density (measured at approximately 1.2% in the lumbar spine at 2 years) is much less than the increase in bone density seen with bisphosphonates (measured at approximately 6% at 2 years with alendronate).
While results of the Early Breast Cancer Trialists’ Collaborative Group overview analysis did suggest a modest though significant reduction in cardiac events, trials like the National Surgical Adjuvant Breast and Bowel Project (NSABP) P-1 and the “Myocardial infarction risk and tamoxifen therapy for breast cancer” have failed to show a benefit in reduction of cardiovascular events in postmenopausal women with coronary artery disease. The current consensus is that, in postmenopausal women both with and without coronary artery disease, the use of tamoxifen does not have a significant impact on cardiovascular morbidity and mortality.
References:
American College of Obstetricians and Gynecologists. Tamoxifen and endometrial cancer: ACOG Committee Opinion 336. ACOG June 2006;Washington, DC.
Braithwaite RS, Chlebowski RT, Lau J. Meta-analysis of vascular and neoplastic events associated with tamoxifen. J Gen Intern Med. 2003;18:937.
Curtis RE, Freedman DM, Sherman ME, et al. Risk of malignant mixed mullerian tumors after tamoxifen therapy for breast cancer. J Natl Cancer Inst. 2004;96:70.
Levine MN. Adjuvant therapy and thrombosis: How to avoid the problem? Breast. 2007;16(Supplement 2):169-174.
Powles TJ, Hickish T, Kanis, JA. Effect of tamoxifen on bone mineral density measured by dual-energy x-ray absorptiometry in healthy premenopausal and postmenopausal women. J Clin Oncol. 1996:14:78.
Reis SE, Costantino JP, Wickerham DL. Cardiovascular effects of tamoxifen in women with and without heart disease: Breast cancer prevention trial. J Natl Cancer Inst. 2001;93:16.
1E08
Key word: Characteristics of Gastrinomas
Author: Ying Wei Lum, MD
Editor: Anne O. Lidor, MD, MPH
A 48-year-old male presents with persistent peptic ulcers that have been refractory to proton-pump inhibitors. His workup includes a positive secretin stimulation test. His underlying tumor is:
View Answer
Answer: (E) Likely to be sporadic
Rationale:
The clinical scenario describes a patient with a gastrinoma. The secretin stimulation test is a provocative test measuring gastrin levels in response to an intravenous bolus of secretin after an overnight fast. It is positive if gastrin levels increase to greater than 200 pg/mL.
Seventy-five percent of gastrinomas are sporadic; the remainder are associated with MEN 1 syndrome. All other choices in the question are associated with insulinoma.
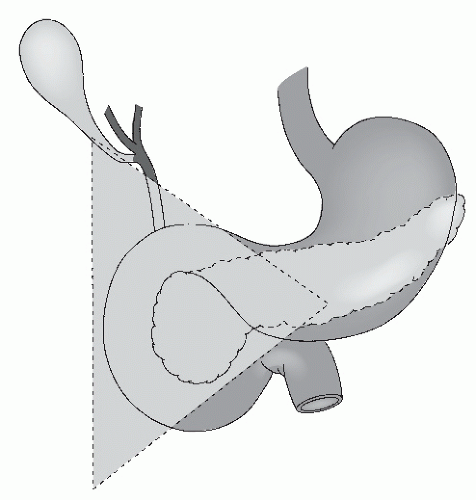
Gastrinomas are more frequently located in the “gastrinoma triangle,” which is bordered by the cystic duct-common bile duct junction, the junction of the second and third portion of the duodenum and the junction between the head and neck of the pancreas.
Gastrinoma | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||
Reference:
Kennedy EP, Brody JR, Yeo CJ. Neoplasms of the endocrine pancreas. In: Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery: Scientific Principles & Practice. 5th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2011.
1E09
Key word: Rate of Nerve Regeneration
Author: Justin B. Maxhimer, MD
Editors: Paul N. Manson, MD, FACS, and Gedge D. Rosson, MD
A 25-year-old male sustains a superficial gunshot wound to his left proximal, lateral thigh, near the anterior superior iliac spine. His initial neurologic examination in the emergency department reveals no motor deficits but numbness in the region of the left lateral cutaneous nerve of the thigh. When should surgery for repair of the suspected nerve injury be performed?
View Answer
Answer: (B) 2 to 3 months
Rationale:
Surgical timing is very important after an injury resulting in nerve damage. Immediate primary repair may be indicated in clean lacerating injuries in which the nerve ends are visible or when clinical examination reveals obvious motor and sensory deficits. Contaminated or complicated transections are best treated by delayed repair. Knife wounds may be explored early—either immediately if there are also some other structures that need to be repaired, or over the next few weeks if there are no other urgent reasons to take the patient to the operating room. Ballistic injuries generally have surrounding damage and are best explored 2 to 3 months after the injury. In gunshot wounds, nerve injury typically results from the blast effect rather than the trajectory of the projectile itself. Hence, gunshot wounds are considered blunt rather than sharp nerve injuries. It is for this reason that a delayed repair (i.e., 2 to 3 months) is recommended.
For injuries to motor nerves, repair should be performed within 3 to 6 months to give the best chance for the axons to regenerate all the way to the motor endplates before they atrophy. For injuries to sensory nerves, repair can actually be performed at any time, as the sensory end organs can be reinnervated many years later.
Sunderland described three fundamental types of nerve injury: (1) A transient interruption of nerve conduction without loss of axonal continuity (i.e., neuropraxia, conduction block), (2) transection of axons (or conditions leading to loss of axonal integrity) with preservation of the endoneurium during wallerian degeneration (i.e., axonotmesis), and (3) complete disruption of the nerve fiber with loss of the normal architecture (i.e., neurotmesis). The third level of injury can be further subdivided to include perineurial disruption (class IV injury) or epineurial transection (class V injury); all injuries that include neurotmesis may result in aberrant regrowth of axons into the wrong endoneurial tubes.
The response of the injured nerve in the first 12 to 48 hours includes wallerian degeneration, which is degeneration of the distal axon to the motor endplate and of the proximal axon to the first node of Ranvier, axonal edema, and retraction of myelin. From 48 to 72 hours, the axons break into twisted fragments and by the second week after injury, all traces of the axon are usually lost. The distal nerve fibers can be stimulated for approximately 72 hours after injury, an essential time frame to consider when contemplating exploration of traumatic nerve injuries, particularly for small, critical motor nerves such as the facial nerve branches. Macrophages are mobilized to phagocytize debris along the nerve and Schwann cells contribute to this activity. However, the main role of the Schwann cells is to guide regeneration by forming dense cellular cords (i.e., Büngner bands) along the site of the degenerating axon. These bands provide conduits for axons once regeneration ensues.
Axonal regeneration generally occurs in four phases. In the initial phase, the neuron recovers, the axonal growth commences, and the axons reach the injured zone. In the second phase (scar delay), the axons must traverse the scar tissue at the site of injury. During the third phase, the axons propagate beyond the site of injury to reach the peripheral target where functional recovery (fourth phase) occurs with restoration of normal patterns of conduction. The duration of the regenerative process varies and may require 6 to 18 months, depending on the length of the nerve and the site of the lesion. Although the commonly quoted regeneration rate is 1 mm/day, this figure varies considerably and can be used only as a rough estimate. Occasionally, very early signs of recovery may be present, which are thought to be due to so-called pioneer axons, which quickly navigate the pathway to the target tissue ahead of most nerve fibers.
References:
Cheng ET, Utley DS, Ho PR, et al. Functional recovery of transected nerves treated with systemic BDNF and CNTF. Microsurgery. 1998;18(1):35-41.
Hebert-Blouin M, Spinner RJ. Nerve injury and repair. In: Cameron JL, Cameron AM, eds. Current Surgical Therapy. 10th ed. Philadelphia, PA: Mosby; 2011:648-656.
Myckatyn TM, MacKinnon SE. Microsurgical repair of peripheral nerves and nerve grafts. In: Thorne CH, Beasley RW, Aston SJ, Bartlett SP, Gurtner GC, Spear SL, eds. Grabb and Smith’s Plastic Surgery. 6th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2006:73-83.
Sunderland S. The intraneural topography of the radial, median and ulnar nerves. Brain. 1945;68:243.
1E10
Key word: Etiology of Post Femoral-Tibial Arterial Bypass Swelling
Author: Eric S. Weiss, MD, MPH
Editors: G. Melville Williams, MD, FACS, and Christopher J. Abularrage, MD
A 72-year-old man with a history of diabetes and smoking presents with a 2-day history of excruciating pain in the right lower extremity. The patient states that the pain started while he was sitting in a chair, and that, unlike other pains he has had in the leg before, it was not relieved by elevation of the extremity. Physical examination shows a pale, cool, pulseless, and numb right foot and the calf is quite tender. No pedal Doppler signal is obtainable. The patient is taken to the operating room where on-table angiogram reveals occlusion of the superficial femoral artery. A right femoral below-knee popliteal bypass is performed with restoration of the pulses. Postoperatively in the surgical intensive care unit, the resident notices severe swelling of the right lower extremity and loss of the dorsalis pedis pulse. The most likely etiology of the edema is:
View Answer
Answer: (C) Acute reperfusion injury
Rationale:
Severe acute lower extremity occlusive disease is a limb-threatening emergency, and prompt revascularization is essential. However, the 2-day history of an insensate foot in this patient followed by restoration of his pulses renders him a perfect candidate for compartment syndrome, the dreaded culmination of a severe reperfusion injury. Reperfusion injury is caused by oxygen-free radical release after return of pulses, and is the most common cause of post revascularization swelling. Most surgeons would have performed a four-compartment fasciotomy at the time of the primary procedure to accommodate the anticipated swelling. Barring this, it is important to be diligent in assessing for compartment syndrome in the early postoperative period. The primary sign of compartment syndrome is pain, although this assessment can be difficult in the early postoperative period. When faced with the scenario described above, the intensive care resident should immediately measure the pressure in all compartments of the leg. Emergent four-compartment fasciotomy in the face of elevated compartment pressures can save the limb. Incidentally, one should not be fooled by the presence of intact distal pulses in the presence of pain and swollen limbs in a setting suggestive for compartment syndrome; loss of pulses is one of the late findings in patients with critically elevated compartment pressures.
References:
Brant-Zawadzki P, Craig-Kent K. Femoropopliteal occlusive disease. In: Cameron JL, Cameron AM, eds. Current Surgical Therapy. 10th ed. Philadelphia, PA: Mosby; 2011:779-782.
Gourgiotis S, Villas C, Germanos S, et al. Acute limb compartment syndrome: A review. J Surg Educ. 2007;64(3):178-186.
Whitesides TE, Haney TC, Morimoto K, et al. Tissue pressure measurements as a determinant for the need of fasciotomy. Clin Orthop Relat Res. 1975;113:43-51.
1E11
Key word: Treatment of Atypical Ductal Hyperplasia of the Breast
Author: Robert A. Meguid, MD, MPH
Editors: Theodore N. Tsangaris, MD, and Mehran Habibi, MD, MBA
A 47-year-old woman undergoes core-needle biopsy of a lesion found on routine mammography in the lower, outer quadrant of her right breast. Pathology is read as atypical ductal hyperplasia (ADH) of the breast. What is the most appropriate next step in this patient’s management?
View Answer
Answer: (B) Excisional biopsy with wire localization
Rationale:
ADH is defined as: (1) A lesion that has some but not all of the histologic features of DCIS; (2) a lesion with all the features of DCIS but <2 mm in greatest dimension; (3) a lesion with all the features of DCIS but involving only two duct spaces. ADH is found in 31% of biopsies for mammographic calcifications and in 4% of benign breast biopsies.
ADH on core-needle biopsy is associated with a 20% to 25% occurrence of ductal carcinoma in situ (DCIS) and an overall relative risk of 4% to 5% for developing any invasive breast cancer compared to age-matched women of average risk. Therefore, it is important to excise the region of concern for further pathologic examination in the event that malignancy is present. Excisional biopsy following wire localization is the appropriate management of ADH.
Of note, core-needle biopsy has low false-negative rates (<2%), comparable to those for excisional biopsy. When core-needle biopsy reveals benign processes with concordance, there is no need for further surgical follow-up.
Excisional biopsy with wire localization is a diagnostic procedure. Mastectomy or lumpectomy with sentinel lymph node biopsy are therapeutic and should be utilized when the diagnosis of cancer is made. They are inappropriate procedures for ADH. A patient whose excisional biopsy confirms only ADH should be closely followed.
References:
Hatmaker AR, Meszoely IM, Kelly MC. Surgical management of carinoma in situ and proliferative lesions of the breast. In: Fischer JE, Bland KI, eds. Mastery of Surgery. 5th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2007:522-523.
Kass R, Lind DS, Souba WW. Breast, skin and soft tissue. In: Souba WW, ed. ACS Surgery: Principles and Practice. New York, NY: WebMD; revised December 2005. Accessed April 9, 2007. Online Edition.
Lind DS, Smith BL, Souba WW. Breast complaints. In: Souba WW, ed. ACS Surgery: Principles and Practice. New York, NY: WebMD; revised June 2004. Accessed June 9, 2007. Online Edition.
1E12
Key word: Radiation Associated with Thyroid Cancer
Author: Robert A. Meguid, MD, MPH
Editor: Alan P.B. Dackiw, MD, PhD, BSc, BSc(Med), FACS, FRCSC
A 34-year-old male Ukrainian immigrant is seen in clinic for a right-sided thyroid nodule, which shows no uptake on technetium scan. In 1986, he was living near the Chernobyl nuclear reactor during its melt-down. Given this history and probable etiology, what is the most likely diagnosis of his thyroid nodule?