Ectopic Pituitary Adenoma
Lester D. R. Thompson, MD
Key Facts
Terminology
Benign pituitary gland neoplasm occurring separately from and without involvement of sella turcica (a normal anterior pituitary gland)
Clinical Issues
Very rare in ectopic sinonasal tract locations
Sphenoid sinus > > > nasopharynx or nasal cavity
Mean: 50 years
Female > Male (2:1)
Presents with space-occupying effects or endocrine abnormalities
Complete surgical removal, followed by medical/hormone manipulation
Image Findings
Intrasphenoidal mass with erosion of sellar floor
Early, intense, but heterogeneous enhancement
Microscopic Pathology
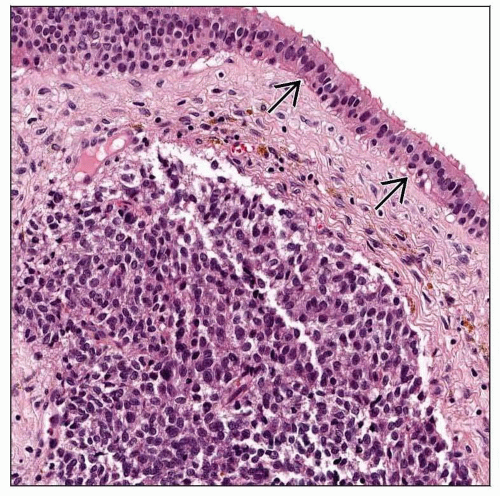
Submucosal location of unencapsulated tumor
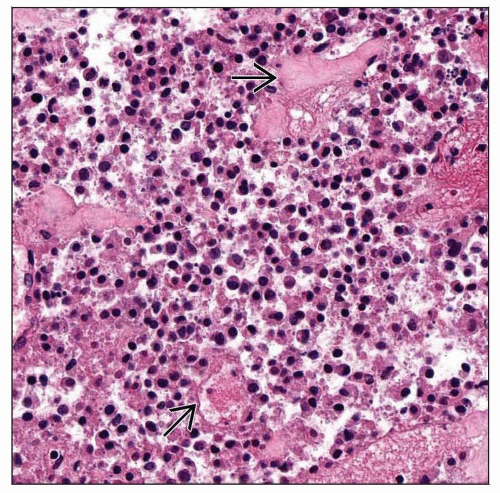
Tumors arranged in many patterns
Tumor groups separated by delicate fibrovascular septae
Monotonous population of round to polygonal epithelial cells
Ancillary Tests
Positive: Keratin, chromogranin–A &/or –B, synaptophysin, CD56, NSE, specific hormones
Top Differential Diagnoses
Olfactory neuroblastoma, Ewing/PNET, neuroendocrine carcinoma, squamous cell carcinoma, lymphoma, meningioma
TERMINOLOGY
Definitions
Benign pituitary gland neoplasm occurring separately from and without involvement of sella turcica (a normal anterior pituitary gland)
Direct extension from intrasellar neoplasm is much more common (seen in about 2% of pituitary tumors) and must be excluded
ETIOLOGY/PATHOGENESIS
Pathogenesis
Anterior pituitary primordium appears at about 4 weeks of embryogenesis
During 8th developmental week, pituitary divides into sellar and pharyngeal parts
Supradiaphragmatic attachment to pituitary stalk
Cephalic invagination of Rathke pouch (infrasellar)
Migration into sphenoid or pharynx can be seen, often along craniopharyngeal canal
Ectopic pituitary adenomas are thought to be derived from these embryologic remnants along the migration path of Rathke pouch
Leptomeningeal locations are common but still intracranial
Fully functional tissue in these ectopic locations is compatible with normal life
Pharyngeal pituitary begins hormone function at 17th-18th week, up to 8 weeks after sellar pituitary
CLINICAL ISSUES
Epidemiology
Incidence
Pituitary adenomas account for 10-15% of intracranial neoplasms
Very rare in ectopic locations within upper aerodigestive tract
Age
Wide range: 16-84 years
Mean: 50 years
Gender
Female > Male (2:1)
Site
Sphenoid sinus > > > cavernous sinus > 3rd ventricle > nasopharynx, nasal cavity, clivus > > petrous temporal bone
Must exclude “invasive sellar” tumors or direct extension from intracranial primary
Intact pituitary sellar is usually required
Presentation
Space-occupying effects
Nasal obstruction or airway obstruction
Headaches
Bloody nasal discharge or epistaxis
Cerebrospinal fluid leakage (clear fluid)
Visual field defects (diplopia)
Endocrine abnormalities seen in around 50% of patients
Cushing disease (adrenocorticotrophic hormone [ACTH]) most common
Acromegaly (growth hormone [GH])
Hyperthyroidism (thyroid-stimulating hormone [TSH])
Amenorrhea, hirsutism, impotence (prolactin [PRL])
Diagnosis unsuspected in functionally silent tumors
Chronic sinusitis
Rarely, cranial nerve(s) paralysis
Laboratory Tests
All ectopic hormones can be measured serologically or via stimulation/suppression testing
ACTH, GH, TSH, prolactin, cortisol
Releasing hormones can also be measured
Treatment
Surgical approaches
Surgery is treatment of choice but only if completely removed
Transnasal/transsphenoidal approach
Drugs
Medical/hormonal manipulation
Dopamine-agonists (bromocriptine), somatostatin analogs (octreotide), corticosteroids (hydrocortisone, prednisone), thyroxine
Radiation
Stereotactic radioablation, usually for larger or incompletely removed tumors
Conventional radiation therapy
Prognosis
Excellent prognosis with control of endocrine abnormalities after complete surgical resection
Morbidity associated with hormonal manifestations and local invasion (bone or cranial cavity extension)
Recurrence may develop in large tumors
Malignant transformation is exceptionally rare
Metastases are not reported
IMAGE FINDINGS
Radiographic Findings
Thin section MR (with and without contrast) or CT yields best results
Intrasphenoidal mass with erosion but usually not expansion of sellar floor
Sella may be involved by upward extension, although usually normal
Usually show early, intense, but heterogeneous enhancement
CT and MR define extent and location of tumor
Diagnostic procedures usually suggest another type of neoplasm
Chordoma, nasopharyngeal carcinoma, or metastatic tumor
MR Findings
T1WI: Rounded, isointense mass within sphenoid sinus; usually fills sinus; partially empty sella
Post contrast, mass will strongly enhance, although can be heterogeneous
T2WI: Isointense mass within sphenoid
FLAIR technique results in hyperintense signal
CT Findings
Variable attenuation, isodense with gray matter
Rarely, hemorrhage and calcification can be seen
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree