Drug-related Acute Hepatitis
Sanjay Kakar, MD
Key Facts
Etiology/Pathogenesis
2 chief mechanisms: Intrinsic and idiosyncratic
Herbal and botanical drugs are important but often overlooked cause of hepatotoxicity
Clinical Issues
Classified into hepatitic, cholestatic, or mixed based pattern of enzyme elevation
DILI with autoimmune markers can be indistinguishable from de novo AIH
Symptomatic and biochemical improvement in most cases on withdrawal of drug
Minority of cases progress to chronic hepatitis and rarely cirrhosis
Jaundice, high AST levels, and preexisting chronic liver disease are adverse prognostic factors
Microscopic Pathology
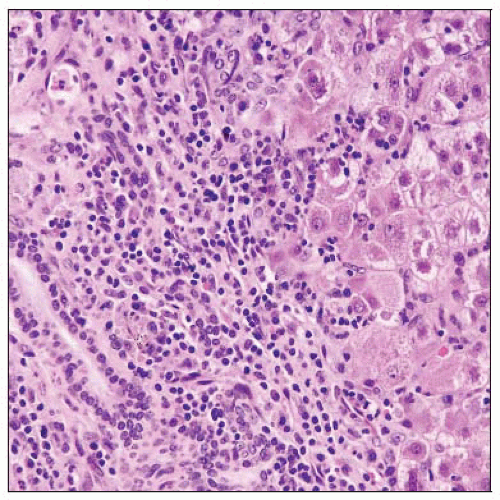
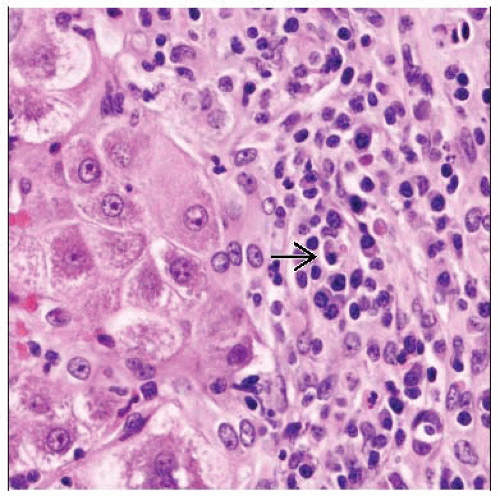
Most medications produce inflammationpredominant pattern
Most toxins & a few medications like acetaminophen produce necrosis-predominant pattern
Concomitant bile duct injury, eosinophils, granulomas, perivenular necrosis, and cholestasis out of proportion to hepatocellular injury suggest DILI, but none of these are specific
Top Differential Diagnoses
Inflammation-predominant pattern: Acute viral hepatitis, autoimmune hepatitis, Wilson disease
Necrosis-predominant pattern: Herpes/adenoviral hepatitis, ischemic necrosis, acute venous outflow obstruction
TERMINOLOGY
Abbreviations
Drug-induced liver injury (DILI)
ETIOLOGY/PATHOGENESIS
Two Chief Mechanisms
Intrinsic hepatotoxicity
Predictable, dose-dependent hepatocellular damage by drug or its metabolite
Industrial, household, or environmental toxins
Typical histological feature is necrosis with negligible inflammation
Idiosyncratic hepatoxicity
Majority of adverse drug reactions fall in this category
Further classified into metabolic and immunological categories
Metabolic: Drug is metabolized into toxic metabolite in predisposed individuals
Immunological: “Drug allergy” or hypersensitivity following sensitization to drug
Typical histological feature is inflammationpredominant liver injury
Herbals/Botanicals
Important but often overlooked cause of hepatotoxicity
Not regulated by Food and Drug Administration and hence not subject to rigorous testing
Nearly 20% of American adults have used herbal remedies, and more than 5 billion dollars are spent on these annually
Contaminants in herbal supplements, including heavy metals such as arsenic, cadmium, lead, or mercury, can also lead to liver toxicity
CLINICAL ISSUES
Presentation
Clinical patterns of injury classified based on pattern of liver enzyme abnormalities
Hepatitic
Acute hepatitis with autoimmune markers may mimic autoimmune hepatitis (AIH)
May have features of hypersensitivity like rash, arthralgia, and peripheral eosinophilia
Progression to chronic hepatitis with fibrosis and even cirrhosis can occur
Cholestatic
Mixed
Classified into acute or chronic based on duration of injury
Establishing drug as causative agent is key
Temporal profile of onset of liver dysfunction is crucial
Liver toxicity may manifest weeks or months after drug ingestion and even after drug has been stopped
Systematic literature search for each drug that patient has been taking is necessary
If observed and reported patterns of clinical and histological injury are similar, case for DILI is strengthened
Rechallenge can help confirm drug etiology but is rarely done
Laboratory Tests
Measurement of serum levels of drug or its metabolite can be helpful in diagnosis (e.g., acetaminophen toxicity)
Antinuclear &/or antismooth muscle antibodies may be present
Transaminase elevations may be marked
Treatment
Drug withdrawal
Steroids may be necessary
Prognosis
Symptomatic and biochemical improvement in most cases on withdrawal of drug
Liver enzymes can remain elevated for up to several months after discontinuation of drug
Minority of cases progress to chronic hepatitis, and rarely, cirrhosis (despite drug withdrawal)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree